The history of the Vitus Private Clinic
Physicists and doctors develop gentler therapy for prostate cancer
I am Michael Stehling, physician, radiologist and physicist. The VITUS Prostate Center was founded by me in 2011.
The first decades of my career were spent in the development and clinical implementation of magnetic resonance imaging. I was fortunate to be initially sponsored by Prof. Ian Isherwood in Manchester, UK, after studying medicine and physics. Prof. Isherwood introduced me to the physicist and later Nobel Prize winner for medicine, Sir Peter Mansfield, in Nottingham. Peter Mansfield, one of the two inventors of MRI along with Paul Lauterbur, gave me the opportunity to participate in the technical development of MRI as a PhD student and research assistant.
After stays in Switzerland and at the Siemens Research Laboratory in Erlangen, I then spent two years as a Clinical Fellow at Harvard Medical School. After several years as head of the magnetic resonance imaging section at Klinikum Großhadern, I left the university and started my own ventures.
The foundations for IRE in Germany with support from the USA
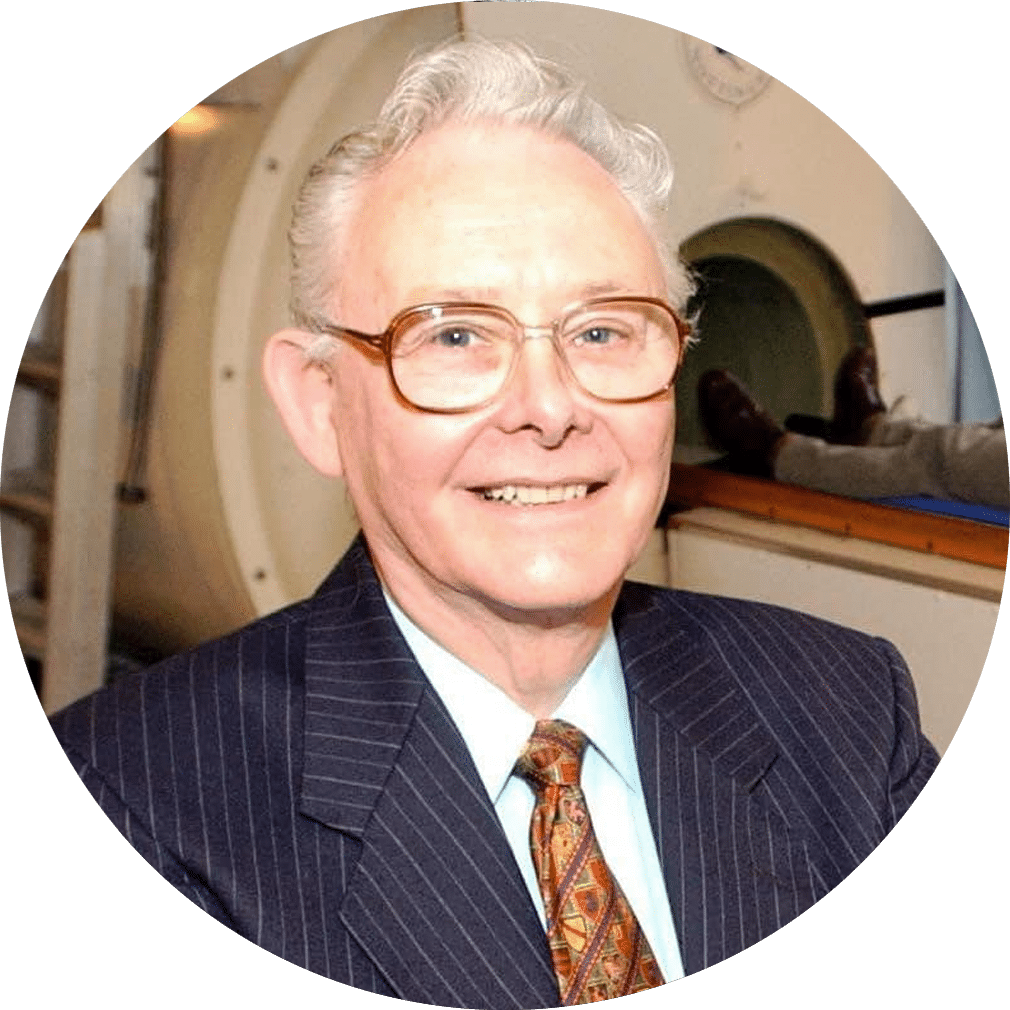
Nobel Prize Laureate 2003
University of Nottingham
The foundation for the VITUS Prostate Center was laid in 2010 during my professorship at Boston University. My friend and mentor Prof. Ducksoo Kim, whom I knew from my days at Harvard Medical School, pointed me one day to a new tissue ablation procedure that supposedly can selectively destroy cells while preserving other tissue components – Irreversible Electroporation, or IRE.
Encouraged by Prof. Kim and the then head of radiology at Boston Medical Center of Boston University, Prof. Alexander Norbash, it was immediately clear to me that we should evaluate this method for its suitability in the treatment of prostate cancer. This is because the prostate is surrounded by delicate structures that are destroyed during conventional treatments such as surgical removal of the prostate and radiation therapy, with serious side effects. We believed that these could be avoided by using the IRE.
At that time, the US company AngioDynamics had just acquired the start-up Onkobionics, along with the first device for tissue ablation with IRE – which was given the product name NanoKnife® at AngioDynamics. I bought two NanoKnifes, one for my practice clinic in Offenbach, a second for Boston University for research purposes. Attempts to start a cooperation with the urology and/or radiology department at the University Hospital Frankfurt am Main had failed. There was no interest in IRE and the NanoKnife® at the clinic.
So we began treating men with prostate cancer using IRE, first in our own radiology institute, the Institute for Imaging Diagnostics, and later in the Prostate Center, the forerunner of the VITUS Private Clinic. The goal was clear: to gently remove cancer cells while avoiding the common side effects of established treatments for prostate cancer, namely impotence and incontinence. This is because IRE’s technique works in such a way that only cells are destroyed, while tissue infrastructure, nerves and vessels are preserved.
My team consisted of two physicists, Enric Günther and Nina Klein, my radiological colleague Dr. Stefan Zapf and myself. We received great support from the very experienced anesthesiologist, Dr. Oliver Grohs, and our nurses at VITUS.
Successful establishment of the VITUS Prostate Center
International and interdisciplinary cooperation in research and clinical application of electroporation techniques
Between 2011 and 2020, we developed IRE and other electroporation techniques to clinical application readiness.
Through close cooperation with the inventor of IRE, Prof. Boris Rubinsky, we were able to perform preclinical studies in experimental animals, both in the USA and in Europe, in addition to basic experiments in the laboratory that helped us to better understand the physical principles of IRE. The Jesús Usón Minimally Invasive Surgery Centre in Spain and the Institutul Clinic Fundeni research facility led by Prof. Popescu in Bucharest, Romania, were ideal platforms for these research projects.
In the experiments, it became clear that IRE is not only IRE, but also has thermal components and produces electrolysis products. These are tissue toxic. Only when these effects are understood and taken into account can safe tissue ablations be performed with IRE and optimal results be achieved.
Many of the techniques we use today in routine clinical practice are based on the findings from these studies. This is the main reason why we use IRE and other electroporation procedures at VITUS Private Clinic differently than most other clinics – and more successfully, with fewer side effects.

Very Unfavorable Climate For Innovation
Germany hinders medical progress
While we were supported by colleagues from abroad and IRE was and is increasingly used for the treatment of tumors there as well, we were met with only criticism from academic institutions and urologists in Germany. Physicians who had no experience with IRE or other focal therapies swung to cautionary experts: IRE was completely unsuitable for treating prostate cancer.
This was inferred in part because a trial of treating lung tumors with IRE yielded poor results – the tumors continued to grow. The conclusion was that the IRE had failed utterly. By means of knowledge at school physics level, however, one can relatively quickly determine that air is an insulator for electric currents. Accordingly, since IRE is based on electric fields and currents, it is no surprise that IRE does not work in the air-filled lung. To dismiss IRE for this reason as a failed attempt at minimally invasive cancer therapy is at the very least premature, and probably a mistake considering the thousands of patients who have already received successful and gentle treatment through this procedure.
It is complicated by the fact that university hospitals claim to place clinical evaluations of novel medical techniques and therapies exclusively in the hands of academic institutions. Such demands impede medical progress, ultimately harming patients who do not have access to improved therapies that have already been developed.
German academic institutions have had ten years to evaluate the IRE – not much has happened to date. Furthermore, it is difficult for patients to get reimbursed for the cost of treatment. Thus, IRE remains a privilege for a few patients who can afford the treatment.
After more and more studies abroad and our own published data indicated that IRE is well suited for the treatment of prostate cancer, the wind is now slowly turning. German university hospitals are also now using IRE in individual cases. So here’s hoping that progress hasn’t stopped completely after all, and that patients will soon have access to a choice of treatments.
