The NanoKnife™ process
Irreversible electroporation (IRE)
The NanoKnife™ tissue ablation procedure is a novel therapy that uses Irreversible Electroporation (IRE) to destroy cells. The surrounding tissue is not injured in the process. Prostate cancer can be treated for the first time with this method in such a way that continence is preserved and there is only a low risk of impotence. In addition, the NanoKnife procedure has a very low likelihood of pain or scarring.
Here at VITUS, we are proud of the pioneering work we have done with the NanoKnife process. We are among the world’s leading experts in the use of IRE in the treatment of prostate cancer.
Through our close collaboration with the inventor of IRE for medical purposes, Prof. Boris Rubinsky of the University of Berkeley in the USA, we have had the opportunity to study and understand IRE at all stages of development, from laboratory to animal studies to human application. Our physicists and physicians are thus among the pioneers and world’s leading experts in electroporation processes – both in the scientific-technical field and in clinical use.
How does IRE work?
Biophysics of the
Irreversible
Elecroporation
Non-thermal tissue ablation by strong electrical pulses
Electroporation processes were already used in the food industry around 1958 by Doevenspeck in Germany1.
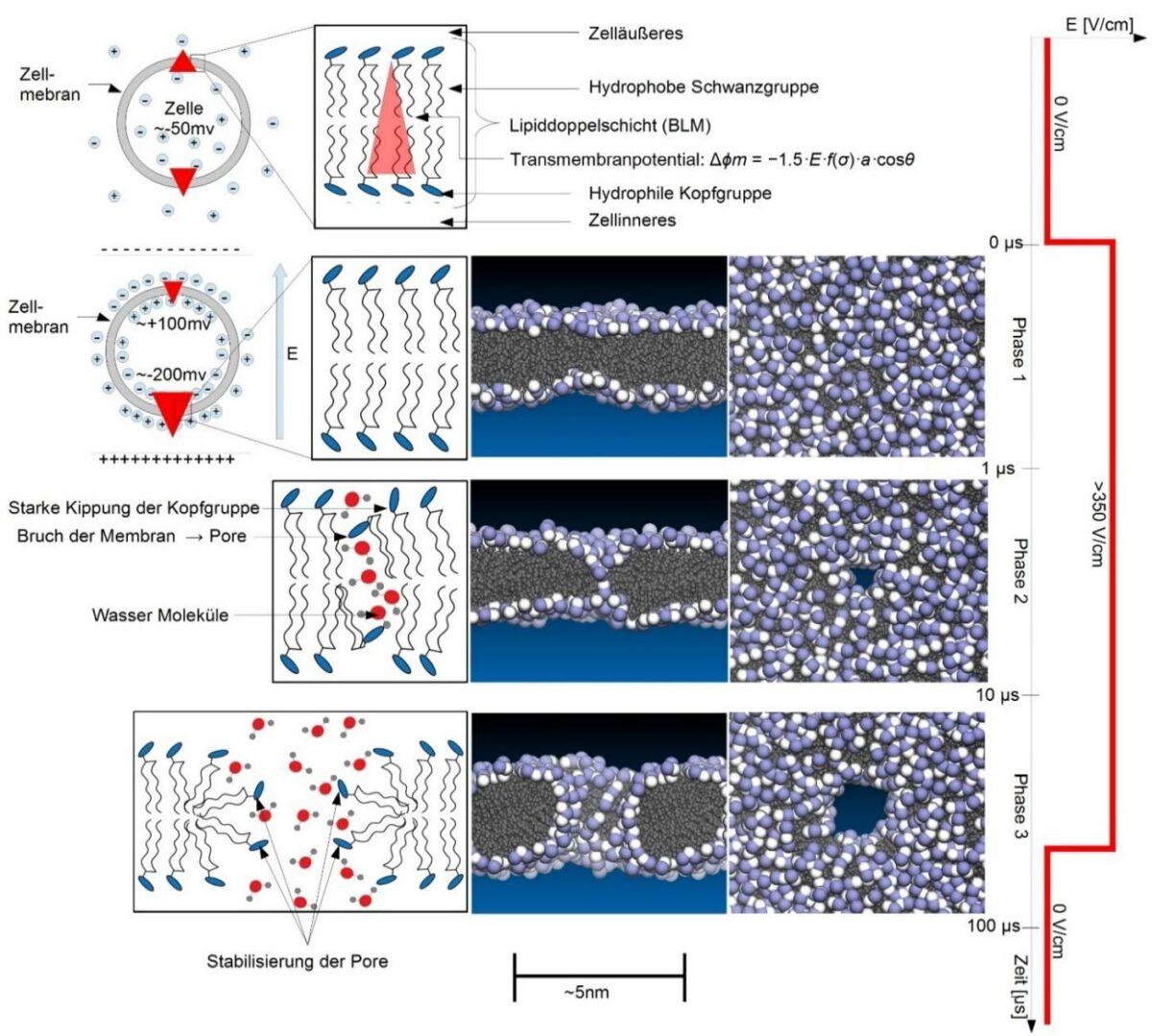
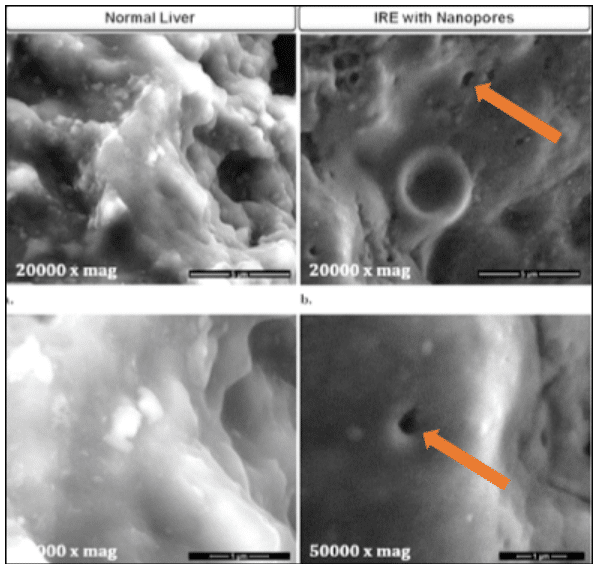
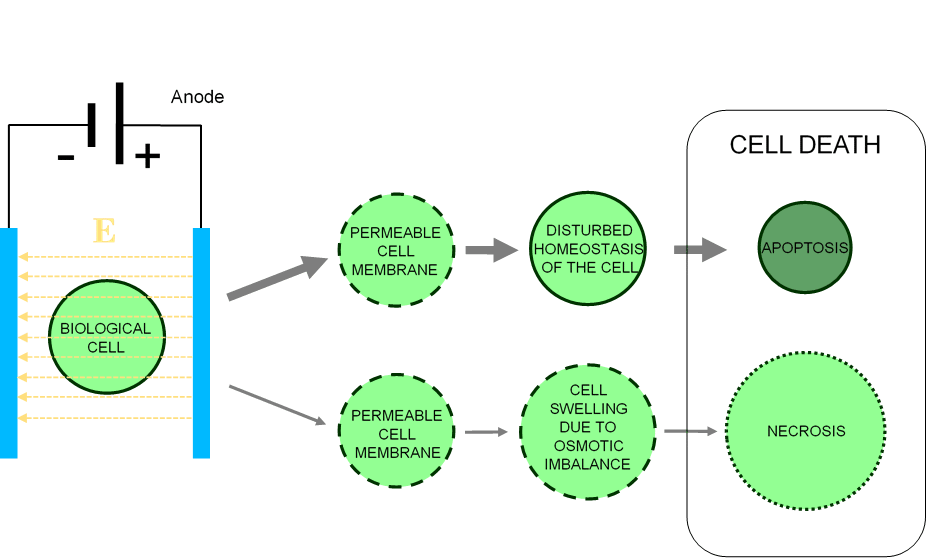
When cells are exposed to strong electric fields, pores (small holes in the cell membrane) form, perforating the cell membrane (Figures 3 and 4). In the case of irreversible electroporation, these pores do not close again. This makes the cell dysfunctional, triggering what is known as apoptosis, a “suicide mechanism” of the cell. Necrosis mechanisms are also involved in cell death by Irreversible Electroporation (see Figure 5).
The electric fields are generated by very short electric pulses, typically 100 microseconds, or 0.0001 seconds long. Because the effect of IRE on tissue is primarily produced by the electrical pulses and not by heat, as in radiofrequency ablation or HiFU (High Energy Focussed Ultrasound), IRE was initially also called non-thermal IRE (NTIRE). While the short duration of the electrical pulses may limit tissue heating, it cannot be largely avoided (see below).
Selective destruction of cells
Preservation of the tissue infrastructure
Compared to other so-called thermal tissue ablation procedures that destroy tissue with heat, particularly radiofrequency (RF) and microwave ablation commonly used on the liver and HiFU (High Enerby Focussed Ultrasound) used in the prostate, IRE offers a number of advantages that make it particularly suitable for the treatment of prostate cancer.
This includes the fact that IRE selectively destroys cells while preserving other tissue components such as fibers and interstitial matrix. The latter is destroyed by thermal ablation procedures, resulting in complete tissue necrosis (melting of the tissue). By preserving the tissue infrastructure, IRE treatment can preserve anatomical structures such as vessels and nerves, and in the prostate area also, for example, the wall of the urinary bladder and the bladder sphincter. This is a prerequisite for avoiding side effects such as impotence and incontinence, which are common with conventional treatments of the prostate.
IRE treatment in prostate cancer:
More than just electroporation
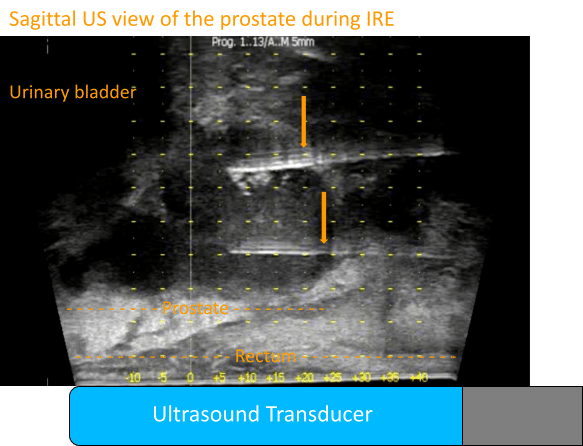
Figure 4 shows an IRE treatment of the prostate as it appears on ultrasound (US). The US probe is located in the rectum (rectal) and depicts the prostate here in longitudinal section (sagittal plane of the body): Headward (cranial) is on the left side of the image, footward (caudal) is on the right side of the image, and the front of the body is at the top. Shown are the prostate and seminal vesicle (star) and part of the urinary bladder. Two IRE electrodes can be seen (arrows) that were initially placed in the caudal portion of the prostate, also called the apex.
During the application of the IRE pulses, muscle contractions occur, which can be seen as jerky movements of the prostate.
The loss of imaging of the prostate in the US that then takes place is striking. The electrical pulses cause electrolysis with gas formation. The gas bubbles scatter and reflect the ultrasound, so imaging of the anatomical structures is no longer possible.
The gas is initially deposited in the connective tissues and is only slowly absorbed. This makes it difficult to reposition the electrodes, which is necessary to treat the cranial portion of the prostate, also called the base.
IRE is more than just
irreversible
Electroporation:
Gas formation indicates electrolysis
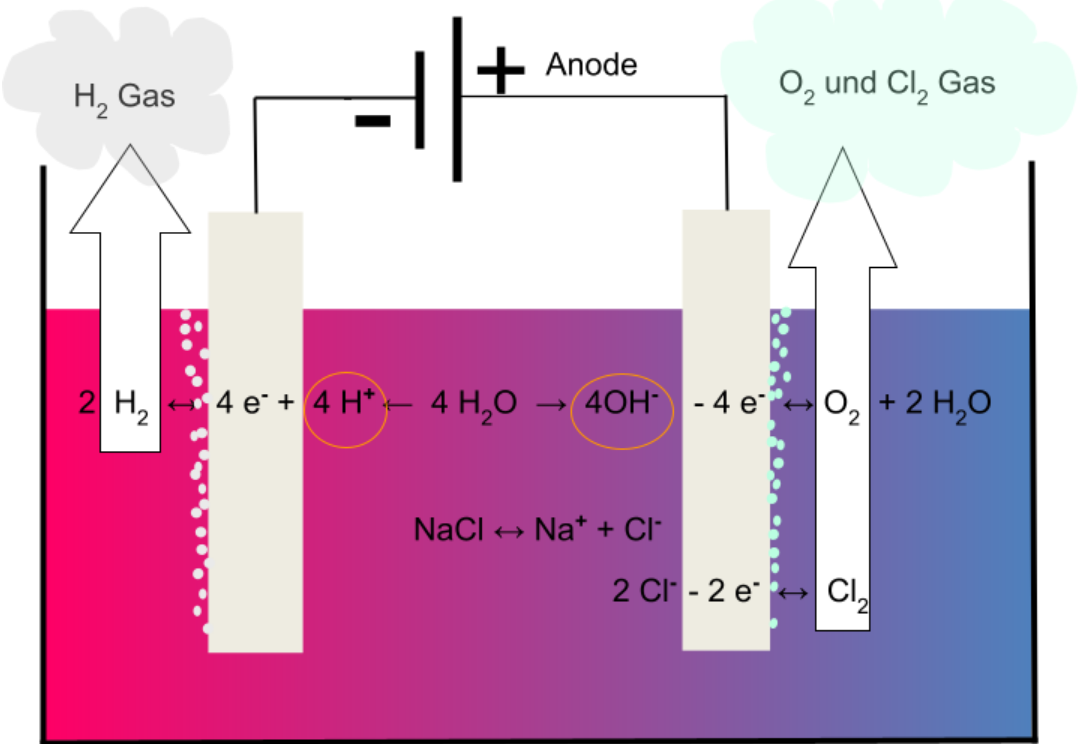
In irreversible electroporation, short electrical pulses of about 100 µsec duration and with voltages up to 3000 V are repeatedly applied. These result in corresponding currents of up to 50 A strength between the IRE electrodes. Since tissues consist largely of water with salts dissolved in it, this leads to electrolysis²,³. This component of irreversible electroporation was not known at the time IRE was introduced into clinical use.
Thermal aspects of the “non-thermal” IRE
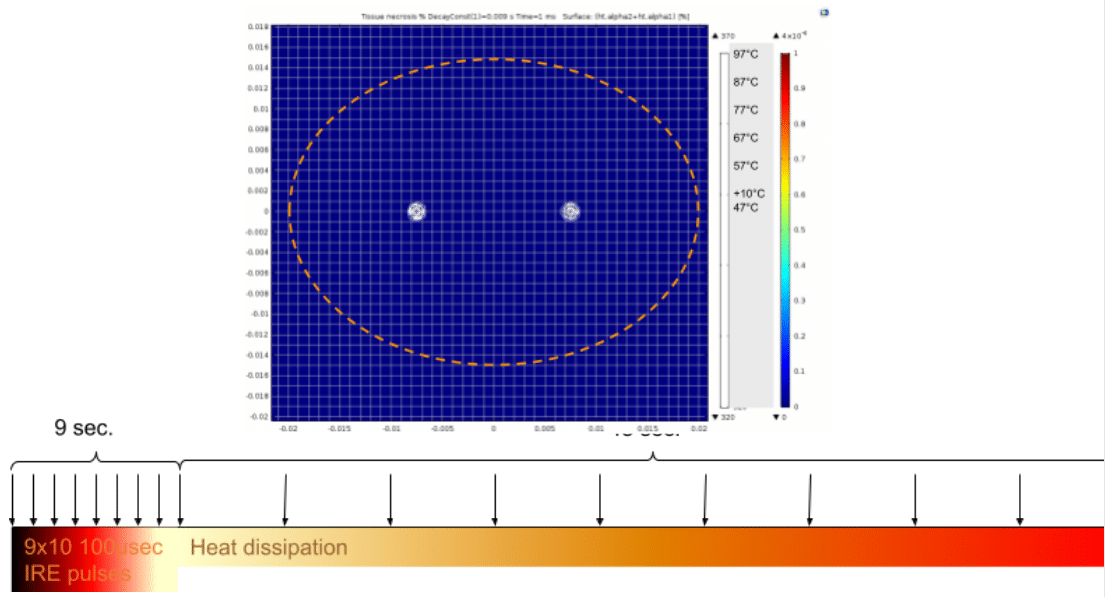
Another aspect to consider in IRE ablations is the joule heat generation around the electrodes. This heat evolution is due to the flowing current and is as unavoidable in IRE applications as electrolysis. The heat evolution is proportional (proportionality constant K) to the square of the current I, the resistance of the fabric R, and the on-time of the current t: H = k ∙ I2 ∙ R ∙ t.
Computer simulations performed by us show the heat development around IRE electrodes (Figure X): The left scale shows the heating in degrees Celsius, the right colored scale shows the degree (percentage) of thermal tissue ablation. 100% tissue destruction by heat is achieved in a circle (two-dimensional simulation) with a diameter of approx. 3.5 mm, partial thermal damage of the tissue in a circle with a diameter of 5 mm around the IRE electrode.
These effects must be considered in an IRE treatment to avoid damage from heat exposure but also excessive electrolysis. Both elements are capable of destroying critical anatomical elements such as the bladder sphincter, neurovascular bundles, and/or the wall of the rectum. Many IRE users are still unaware of these connections today.
The right clinical application
The clinical application of IRE requires an understanding of the physics of the procedure
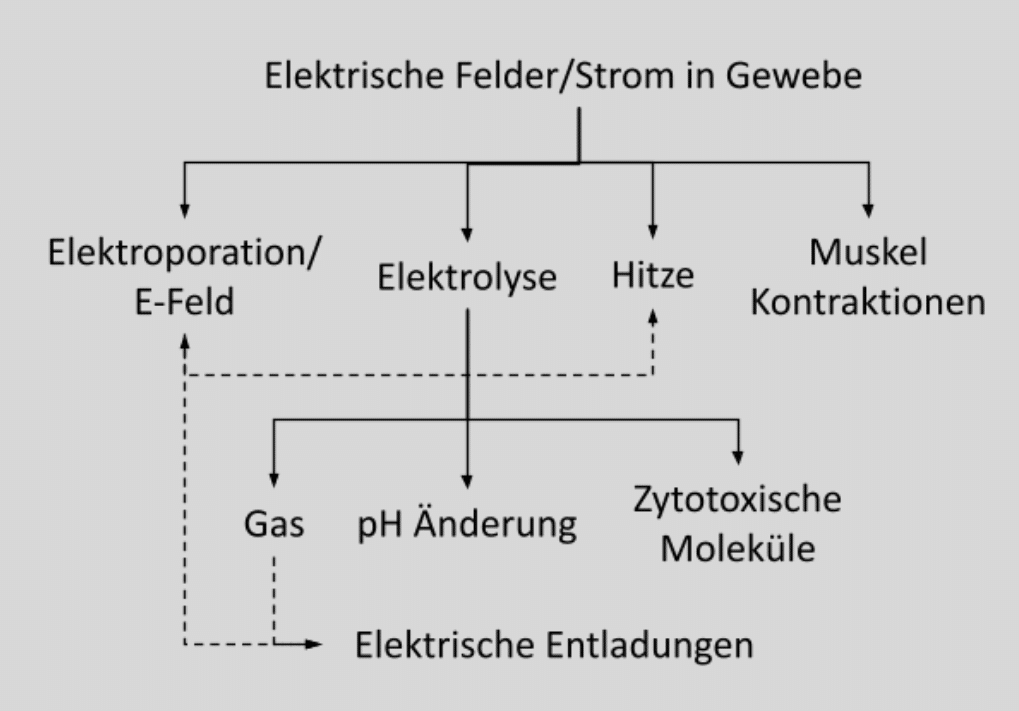
IRE is not just irreversible electroporation but an interplay of complex physical processes involving electrolysis and heat generation. These effects, which go beyond electroporation, depend on tissue ablations with a larger number of electrodes not only on the total number of applied electrical pulses but also on their temporal sequence and on the polarity and geometry of the electrodes. Ignorance of these relationships can result in damage to critical anatomic structures such as the neurovascular bundle, rectum, and bladder sphincter.
While we at VITUS Private Clinic have been able to almost completely eliminate these undesirable side effects through close collaboration between physicists and physicians, publications from other institutions that have used IRE to treat prostate cancer show that IRE can cause significant harm in the wrong hands. Comprehensive user training, especially regarding the technical and physical aspects of IRE, would therefore be desirable. The figure depicts the various physical effects of IRE and how they interact.
Thermal effects, which may lead to “cooking” of tissues near of the electrodes, are also mandatory to consider in the clinical application of IRE. Positioning the electrodes outside the prostate, as is the case with brachytherapy grid placement, thus inevitably leads to destruction of the neurovascular bundles and resulting erectile dysfunction.
Muscle contractions are another issue to watch for in the clinical use of IRE. In particular, when using a brachytherapy grid to position the electrodes, muscle contractions can cause significant displacement of the electrodes by up to 1.5 cm, which may result in damage to the bladder sphincter and other important anatomical structures.
