Irreversible
electroporation – IRE
The NanoKnife™ process
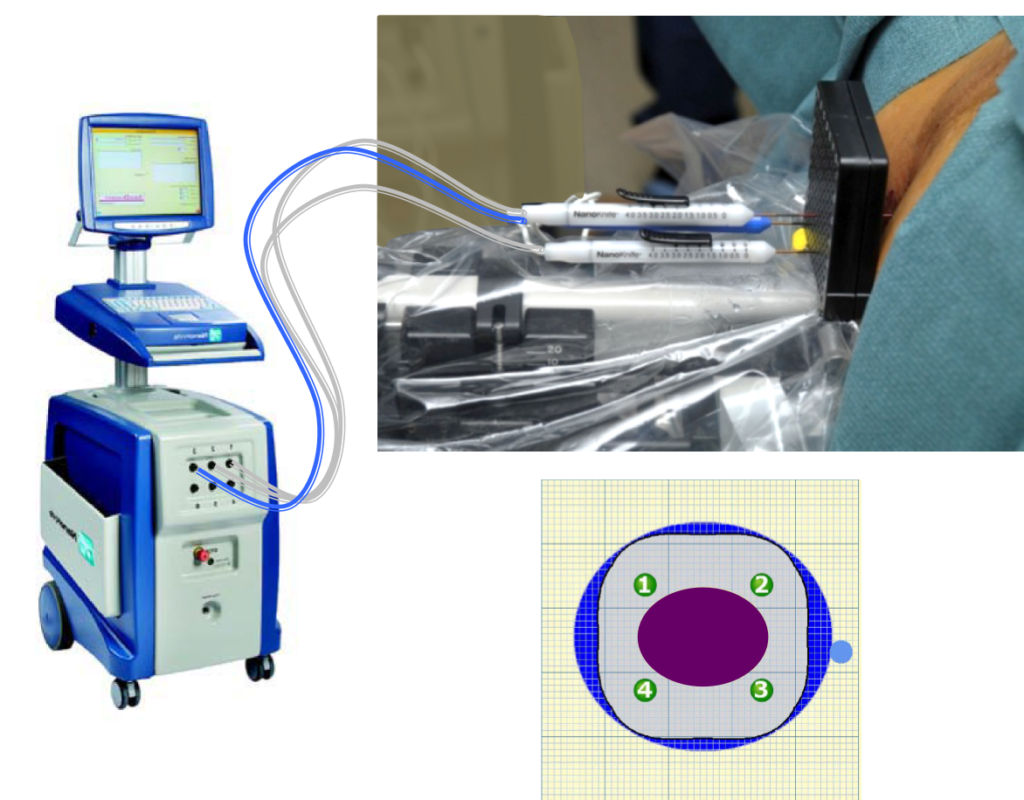
The NanoKnife tissue ablation procedure is a novel therapy that uses Irreversible Electroporation (IRE) to destroy cells. The surrounding tissue is not injured in the process. Prostate cancer can be treated for the first time with this method in such a way that continence is preserved and there is only a low risk of impotence. In addition, the NanoKnife procedure has a very low likelihood of pain or scarring.
Here at VITUS, we are proud of the pioneering work we have done with the NanoKnife process. We are among the world’s leading experts in the use of IRE in the treatment of prostate cancer.
Through our close collaboration with the inventor of IRE for medical purposes, Prof. Boris Rubinsky of the University of Berkeley in the USA, we have had the opportunity to study and understand IRE at all stages of development, from laboratory to animal studies to human application. Our physicists and physicians are thus among the pioneers and world’s leading experts in electroporation processes – both in the scientific-technical field and in clinical use.
Irreversible electroporation (IRE) treatment can avoid side effects such as impotence and incontinence with comparable efficacy
While modern, gentle treatments have long since become established in other areas of medicine, they are still a long time coming in urology. For breast cancer, the entire breast has not been amputated for a long time, but the tumor is removed focally. In renal cell carcinoma, if possible, not the entire kidney is removed, but only the tumor – the healthy part of the kidney is preserved. The prostate is still removed “radically”, i.e. completely, in most cases unnecessarily.
This has changed since the successful introduction of Irreversible Electroporation (IRE) for the treatment of prostate cancer. With IRE, prostate cancer can be focally destroyed, with a lower likelihood of side effects.
The wide range of IRE treatments :
From focal therapy of small carcinomas to a problem solver for unresectable T4 carcinomas.
RE – also known by the product name NanoKnife – enables the gentle treatment of prostate cancer while avoiding impotence and incontinence.
IRE can be used to treat the full range of prostate cancers – from small focal carcinomas to T4 tumors that have already infiltrated the bladder or rectum – inoperable, usually advanced cases.
ADVANTAGES OF THE
NANOKNIFE TREATMENT AT A GLANCE
- One-time treatment on only one day for a 3-day stay
- Highest potency retention rate achieved to date*.
- Statistical 0% Incontinence**, ***
- No surgical incisions
- No aftercare necessary
- No higher recurrence rate than radical procedures**.
- Treatment even after prostatectomy or radiotherapy
- Secondary immunological effects
* Urinary incontinence, as it is called, is the lack or inability of the body to safely store and self-directly empty the contents of the bladder. This leads to involuntary loss of urine. While there are several possible definitions of incontinence, a long-term study of incontinence after prostatectomy** concludes that a reasonable definition of incontinence is when a patient requires 2 or more pads per day 12 months after prostate surgery.
** Sacco E, Prayer-Galetti T, Pinto F, et al. Urinary incontinence after radical prostatectomy: incidence by definition, risk factors, and temporal trend in a large series with a long-term follow-up. BJU Int. 2006;97:1234-41.
*** Syan, Raveen, and Victor W. Nitti. “Post-prostatectomy Incontinence Initial Evaluation.” Urinary Dysfunction in Prostate Cancer. Springer, Cham, 2016. 15-30.
NanoKnife-Technologie
ideal for the treatment of prostate cancer
The NanoKnife process is based on ultra-short pulses that generate strong electric fields. The pulses are 100 microseconds long – i.e. 0.0001 seconds. Compared to standard procedures, this new technology has unique features that make it ideal for treating the prostate.
- Tissue selectivity: Only cells that have a cell membrane, such as cancer cells, are reliably destroyed. All other structures, such as nerves, blood vessels and connective tissue structures, remain intact.
- Ultrasharp edges: With NanoKnife, the area between completely removed and untreated tissue can be measured in micrometers. This clearly sets NanoKnife apart from other treatment methods, such as radiation therapy, heat-based treatments and even surgery. In these methods, the central treatment field is always surrounded by an area where the tissue is unintentionally damaged. Often this is a zone with a diameter of several centimeters.
- Programmed cell death: NanoKnife causes cell death (apoptosis) to occur without causing radiation damage or burns and without forming scars. Current standard methods, such as radiation therapy (proton therapy, brachytherapy, etc.) and heat therapy (HIFU, microwave therapy, etc.), always create a large “toxic” area because the burned tissue is toxic to the body. The result is inflammation and pain with subsequent scarring. All of this prevents or limits further treatments that may be needed in the event of a recurrence.
- Repeatable any number of times: Since IRE treatment does not lead to long-term tissue damage, all other treatment methods (radiotherapy, heat, surgery) can continue without restriction after NanoKnife treatment. In addition, treatment using IRE can be repeated as often as necessary.
- Painless and minimally invasive: because no tissue is damaged by burning or radiation. In addition, only thin needles are used as invasive instruments. Thus, our patients usually hardly notice the treatment.
- Fast and in one session: Even extensive areas can often be treated under general anesthesia in just one session.
- Wide range of possible applications: The treatment of small, early detected prostate tumors is definitely the simplest application of NanoKnife. However, NanoKnife is also a treatment option for inoperable carcinomas that have already breached the prostate capsule, as well as for the treatment of recurrences that occur after radiation therapy, radical prostate removal, HIFU or brachytherapy.
- Immune system: The tumor fragments released during NanoKnife treatment support the patient’s immune system in fighting further prostate tumor cells.
Precision crucial for therapeutic success with NanoKnife
Since 2007, the IRE technique has been approved by the FDA in the USA and CE marking in Europe. This was done because corresponding studies prove that all cells within the treatment area can be killed with this method. In order to achieve this and carry out a successful IRE treatment, two factors are crucial:
- Firstly:
The exact position of the tumor must be known before treatment. - Secondly:
The treatment field must be placed in exactly the right position.
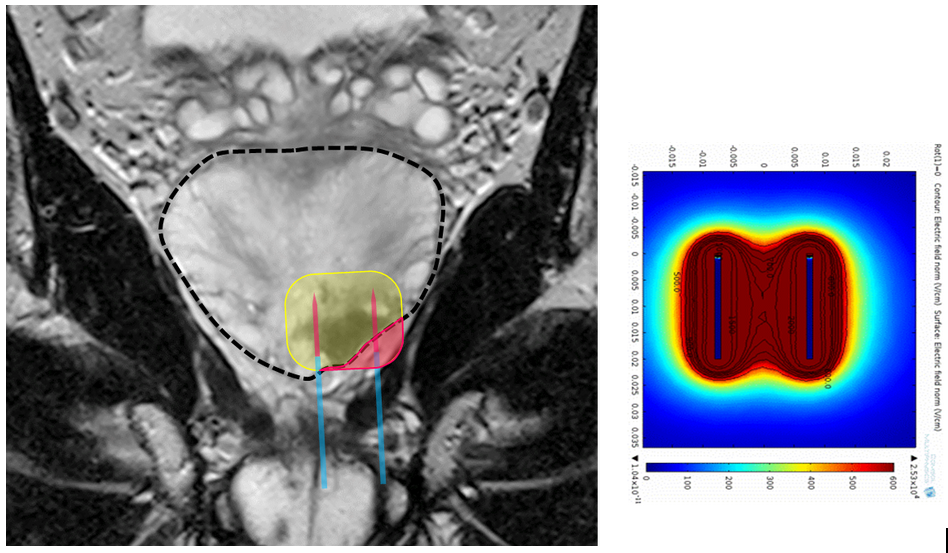
The first condition is met by multiparametric MRI examination, 3D biopsy or, if necessary, other procedures. The second condition is fulfilled by a minimally invasive procedure under general anesthesia. Sterile needles with variable exposure length are inserted. “Exposure length” refers to the area of the needle that exposes the tissue to electrical current. We have experience with this procedure since 2011 and have performed the most prostate treatments worldwide. This makes us one of the leading experts worldwide, while other clinics are just getting started.
Clinical application of IRE in prostate cancer.
Correct Technique decisive for good or bad results
As with many other medical treatments, the technical details of IRE treatment determine its success, i.e., the reliability with which the tumor is destroyed and the side effects triggered by the treatment.
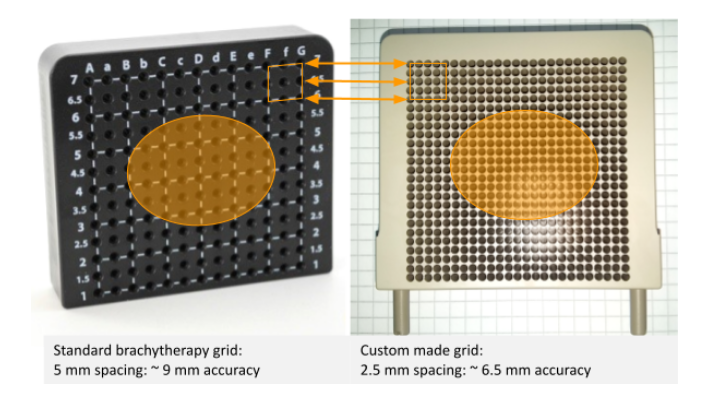
Unfortunately, no technical standards have been established for IRE treatment of the prostate. That is, each physician performs IRE treatments at his or her own discretion using his or her own technique. Most urologists therefore use a grid, also known as a brachytherapy grid, for the placement of the electrodes, which they know from brachytherapy and which is used there for the insertion of the radioactive seeds.
Placement of IRE electrodes with a brachytherapy grid is too imprecise for good treatment results
And that’s where the problems begin. This is because the use of a grid significantly reduces the accuracy with which the IRE electrodes can be placed. This is illustrated below.
Figure 7 shows the problem with using a brachytherapy grid to place the electrodes.
Since the electrodes are made of thin metal rods about 1 mm thick, they are flexible. Leg insertion into the prostate via a hole in the grid, they are more or less bent by the tissue layers of the pelvic floor and deflected from the intended path. With a penetration depth of 6 cm (typical position of the prostate), a bending of only 2 degrees is sufficient for the electrode tip to miss the desired position by 2 mm.
If electrodes are inserted through two adjacent grid holes 5 mm apart, the tips of the electrodes can be positioned in the prostate at a distance of 1 to 9 mm. The probability that they actually achieve a distance of 5 mm is low and would be pure coincidence. With a typical spacing of the electrodes of 15 to 20 mm and a typical size of the prostate of 30 – 40 mm transverse diameter, an inaccuracy of 5 ± 4 mm is completely unacceptable. Insertion of the electrodes via a standard brachytherapy grid is therefore unsuitable.

Die VITUS Methode
Highest accuracy due to manual insertion of the electrodes into the prostate gland
Not only because of the inaccuracy in the X-Y plane of the brachytherapy grid (described in Figures 6, 7 and 8), at the VITUS Prostate Center, we have developed the manual insertion of the electrodes (Fig. 9) perfected. This method allows placement of electrodes with 1 -2 mm precision.
The figures in this section illustrate the advantages of manual electrode placement using the VITUS method.
Figure 9A shows a cross-section through a prostate with a fictitious prostate carcinoma (in magenta) in the right (radiological orientation, left on the image) outer zone. Also shown are the various portions of the neurovascular bundle (NVB), in and on the prostatic capsule as well as extrafascial. More externally located, anatomically poorly defined portions of the NVB are not shown.
Figure 9B shows the superimposition of a standard brachytherapy grid with 5 mm hole spacing over the prostate. According to the technique recommended by the manufacturer Angiodynamics, the electrodes (green dots) should be placed so that the tumor is surrounded by electrodes. The localization of the electrodes results from the nearest grid points, respectively holes in the grid. The figure shows the IRE ablation fields resulting from an application using Grid.
Two facts stand out:
- 1. three of the electrodes are placed outside the prostate capsule, directly in the NVB. This is very likely to lead to NBI violations.
- 2. the total ablation field (the sum of the individual ablation fields) extends far beyond the capsule of the prostate and covers the right NVB.
This leads to unnecessary damage in the right NVB. This is because the electrodes become hot during pulse emission, so they can cause thermal damage if they are in close proximity to sensitive structures. Although these only affect an area of about 1 – 2 mm around each electrode, this is sufficient to damage the right NVB as the electrodes are in direct contact with it. In addition, electrolysis products such as H+ and OH- with an acidic and basic environment are formed around the electrodes during the electrical pulses, which also cause damage to nerves and vessels.

Figure 9 B: Overlay of a standard brachytherapy grid with 5 mm hole spacing over the prostate.
Figure 9 C: IRE ablation fields resulting from the electrode pairs that were inserted manually.
Advantages of manual
electrode placement
in the x-y plane with the
VITUS method
Figure 9C shows the advantages of manual placement of IRE electrodes using the VITUS method. With no predetermined grid points, the electrodes can all be placed within the prostate capsule. Direct damage to the neurovascular bundle (NVB) from heat or electrolysis products emitted from the electrodes is thus avoided.
By placing the electrodes freely, an IRE ablation field can be generated that optimally follows the contour of the prostate so that the tumor (magenta) is safely destroyed, but the NVB is spared.
Advantages of manual electrode placement in the z-plane
(longitudinal direction)
with of the VITUS method
However, electrode placement with the VITUS method brings advantages not only in the x-y plane, but also in the z-direction, the longitudinal axis of the prostate. This is illustrated in Figure 10.
When placing the electrodes through a brachytherapy grid, all electrodes are aligned parallel in the z-direction, except for minor deviations.
However, because the shape of the prostate resembles a pyramid standing on its apex (apex caudal/bottom, base cranial/top), parallel insertion of the electrodes with equal length of the conductive electrode portion results in the caudal/bottom portions of the electrically conductive electrode lying outside the capsule, directly in the NVB, damaging it by heat and electrolysis products (Figure 10 left, red area).
This can be prevented with the VITUS method by inserting the electrodes at an angle, following the prostate capsule. This is only possible manually, i.e. without a grid. By adjusting the “exposure length”, i.e. the electrically conductive electrode portion, it can be achieved that the NBI is protected from heat and electrolysis products (Figure 11). Simulations of the electric field performed by VITUS physicists show that the IRE ablation field in the VITUS method conforms to the prostate capsule even in the third spatial direction (z-direction), thus providing optimal results.