Previous prostate cancer screening
According to experts, conventional prostate cancer screening is useless or even dangerous.
“Palpation of the prostate, the digital rectal examination, or DRU for short, is useless,” says Patric Walsh, head of urology at Johns Hopkins University. In Germany it is still standard and the PSA test has been abolished as a screening test in many countries because an elevated PSA level often triggers an unnecessary biopsy, but a low PSA level does not rule out carcinoma.
So what should men do if they want to protect themselves against prostate cancer? The answer has been clear and scientifically proven for years: Magnetic resonance imaging (MRI) of the prostate can detect or rule out carcinomas with a high degree of certainty.
Talk to us on +49 069 50 50 00 980 or send us an e-mail using the contact form.
Prostata-MRT
The new quality standard in prostate diagnostics.
The PROMIS multicenter study from England1 conducted in 2017 with 576 men was already able to show that MRI of the prostate has a detection sensitivity of 93% for clinically relevant prostate carcinomas, which is almost twice as high as prostate biopsy (TRUS biopsy), which only achieved a sensitivity of 48%.
These data were confirmed by the results of a large multicenter interdisciplinary study in the USA, which included a total of 1500 patients over several years2.
Clinically relevant carcinomas
MRI detects clinically relevant carcinomas with almost 100% certainty.
The researchers demonstrated that multiparametric MRI (mpMRI) of the prostate has a sensitivity for prostate cancer of 94-95%. Of note, MRI was able to exclude clinically relevant carcinomas (Gleason score ≥ 7) with a certainty of 93-97%. If the difficult to detect, almost benign Gleason 6 carcinomas were also taken into account, the negative predictive value was still 87% – much better than with the punch biopsy.
The size and extent of carcinomas in the prostate are also better detected by mpMRI than by punch biopsy, with a sensitivity of 84%. Infiltration of the seminal vesicles and tumor growth exceeding the prostate can be detected with a specificity of 97-98% (Gleason score ≥ 7).
MRT HELPS TO AVOID UNNECESSARY BIOPSIES
Modern examinations using MRI lead to reliable diagnoses.
That magnetic resonance imaging (MRI) can avoid unnecessary biopsies of the prostate has been suspected for years. In 2018, a study by the University of Mainz also provided scientific evidence of this in Germany3. They were able to show that among the 651 men in the study, nearly 40% of biopsies could have been avoided by MRI without missing relevant cancer foci.
In summary, it can be said today that the informative value of prostate MRI is so superior to other procedures that prostate MRI should be performed whenever prostate cancer is suspected.
- If a carcinoma requiring treatment (clinically relevant) is present, this is detected by prostate MRI with a detection sensitivity of 94 – 95%.
- If prostate MRI shows no suspicious findings, clinically relevant carcinoma can be excluded with 93-97% confidence.
- Prostate MRI detects the size and extent of carcinomas in the prostate with 84% accuracy, and capsule-spanning growth with 97-98% confidence.
- Prostate MRI can avoid unnecessary biopsies when PSA levels are elevated or increase the accuracy of biopsies when they are necessary.
Endorectal coil: Necessary or dispensable
In order to generate a signal from which the MRI image can be calculated, the magnetized protons must be “excited”.
Magnetic resonance imaging uses strong magnetic fields (B0) to magnetize protons – hydrogen nuclei – in the human body. Roughly speaking, the protons align themselves parallel to the magnetic field. This magnetization is twice as large at 3 Tesla as at 1.5 Tesla.
To generate a signal from which the MRI image can then be calculated, the magnetized protons must be “excited,” which is done with radio frequency waves of the appropriate frequency: about 64 MHz at 1.5 Tesla, about 128 MHz at 3 Tesla.
The MR signal, more precisely the signal-to-noise (SNR) ratio – increases approximately with the square of the field strength at low field strengths (SNR ~ B07/4), at higher field strengths only linearly (SNR ~ B0).
However, the radio frequency energy required to fully excite the protons and thus achieve full signal for imaging increases with the square of the field strength: SAR ~ B02α2, where α is the strength of the radiofrequency pulse (the “flip angle”). Thus, it is four times higher at 3 Tesla than at 1.5 Tesla!
The absorption of radio frequency (RF) energy heats the body. Therefore, the maximum usable RF energy in commercial MRI scanners used in medicine is strictly limited. If the magnetic field strength B0 increases, the strength of the radio frequency pulses α used for imaging must be decreased.
This only leads to the fact that the higher signal theoretically available at 3 Tesla cannot be used, since it is to be avoided that the patient is damaged by heating.
These restrictions do not apply to the radio frequency coils, antennas that receive the signal needed for imaging. The smaller the so-called RF coil and the closer it is placed to the object to be imaged, the higher the received signal. Since the prostate is posteriorly adjacent to the rectum, a small endorectal coil can be placed directly behind the prostate and doubles4 the signal available for imaging.
In general, therefore, it can be said:
- The image quality required for optimal imaging of the prostate can only be achieved using an endorectal coil.
- The signal gain from 1.5 to 3.0 Tesla is less than the signal gain through an endoractal coil, no matter what the field strength.
- At 3 Tesla, even small amounts of air in the rectum lead to signal deletions in the MRI images, which particularly affect the outer zone near the rectum, where 70 – 80 % of all prostate carcinomas are located – these can thus easily be overlooked.
Recommendation: Have 3 Tesla MRIs of your prostate performed only with an endorectal coil or at least after emptying the rectum by laxative and/or filling the rectum with a susceptibility-neutral fluid – so that you were not “in the tube” for nothing.
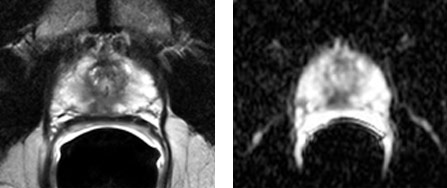
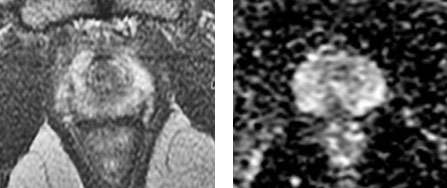
First and second image: MRI images of the prostate taken with a 3 Tesla scanner WITHOUT endorectal coil. The images have a high noise content. The carcinoma (arrow) is not well depicted either on the morphological T2 images (left) or on the functional ADC maps (right).
Third and fourth image: 1.5 Tesla images WITH endorectal coil: The carcinoma is now clearly visualized on all images.
Air in the rectum – prostate gone
The problem of susceptibility artifacts at 3 Tesla.
3 Tesla MRI scanners pose challenges to users that few experts have mastered. It requires a sound knowledge of physics, which most physicians do not have.
For example, most MRI scans of the prostate do not look to see if there is air in the rectum. This is because magnetic fields are sensitive to the different magnetic conductivity (susceptibility) of air and water-containing tissues – as occurs at the interface of the air-filled intestine and the prostate directly in front of it. These so-called susceptibility differences lead to a distortion of the magnetic field and thus to signal cancellations, which particularly affect the outer zone of the prostate near the rectum – where 70 to 80% of all carcinomas are located!

