Nerve-sparing prostatectomy
Wish or reality?
Radical prostatectomy is the standard treatment for prostate cancer. It describes the surgical removal of the entire prostate.
The most common side effects of radical prostatectomy are erectile dysfunction and urinary incontinence. These side effects are caused by damage to important anatomical structures during surgical removal of the prostate.
Erectile dysfunction results from damage to the so-called neurovascular bundle, a network of vessels and nerves that runs in and on the prostate gland and is responsible for the erection of the penis.
Urinary incontinence, the involuntary loss of urine, results from damage to the sphincter of the urinary bladder, which is located below the prostate.
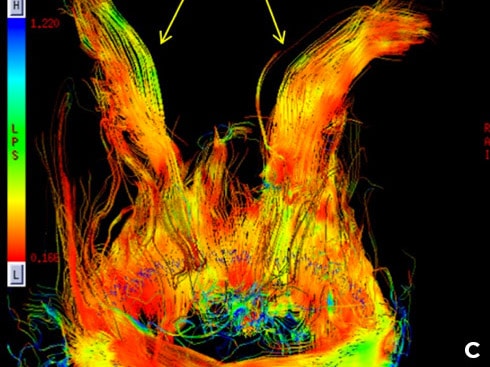
While in simple schematics of radical prostatectomy the neurovascular bundle is usually depicted as a “cable bundle”, in reality it is an extremely complex network of small and tiny vessels and nerves in and on the prostate – and thus cannot be preserved during radical surgery (see Figure 1).



Interfascial or intrafascial nerve-sparing radical prostatectomy.
While in the so-called “interfascial nerve-sparing radical prostatectomy” shown in Figure 2A, the prostate is dissected between the endopelvic fascia (EF), a layer of connective tissue surrounding the prostate, and the prostatic fascia (PF), In the so-called “intrafascial nerve-sparing radical prostatectomy” shown in Figure 2B, the prostate is dissected between the prostatic fascia (PF) and the prostatic capsule (PC).
In this case, the neurovascular bundle (NVB) and the prostatic pedicle (PP) are partially preserved – but just as partially destroyed by the dissection or section plane (dashed line) 1.
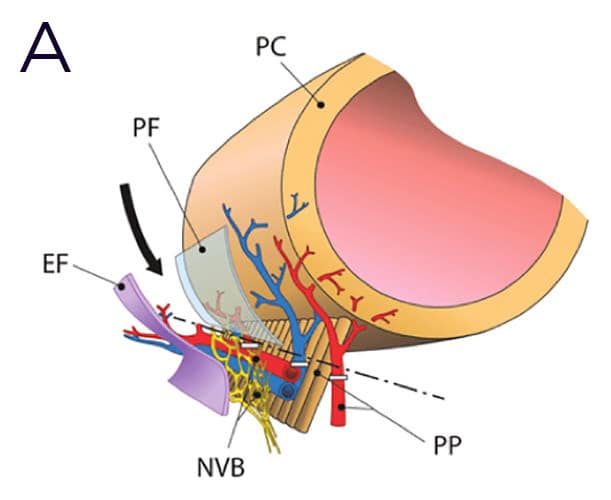
Abbreviations:
PC = prostatic capsule
PF = prostatic fascia
NVB = neurovascular bundle
PP = prostatic pedicle

Impotence and incontinence
Frequent despite nerve-sparing robotic-assisted radical prostatectomy (RARP).
While after conventional robotic-assisted radical prostatectomy (RARP), 70 to 80% of treated men suffer from erectile dysfunction and 20-50% experience incontinence, nerve-sparing RARP reduces these side effects. However, not to zero.
One year after nerve-sparing surgery, 38-40% of operated men still suffer from erectile dysfunction, while 20-40% of men have significant urinary incontinence.
So is nerve-sparing surgery not nerve-sparing enough after all?
There are many reasons for this. Even with nerve-sparing surgery, the neurovascular bundle (NVB) is damaged precisely because it is not a well-defined “wiring harness” that could be easily identified and dissected free. The complex anatomy of the NVB in and on the prostatic capsule makes preservation impossible. In Japan, this was attempted: In operations that lasted up to 10 hours, attempts were made to free the NVB. Without success. Also, impotence rates were about 40%.
Not considered at all in the attempt to preserve the nerves responsible for erection and continence are nerve cords that run outside the neurovascular bundle. These nerve cords, which are variable in their anatomical localization and also play an important role in penile erection and urinary continence, were not anatomically known at all until recently. In addition, they cannot be localized before surgery and thus cannot be spared. Prof. Patric Walsh of Johns Hopkins University has consistently pointed out that the anatomy of the prostate and its surrounding structures is grossly simplified or simply misrepresented in most anatomy books – and little has changed in this regard to date.
Not considered at all in the attempt to preserve the nerves responsible for erection and continence. These are nerve cords that run outside the neurovascular bundle. These nerve cords, which are variable in their anatomical localization and also play an important role in penile erection and urinary continence, were not anatomically known at all until recently. In addition, they cannot be localized before surgery and thus cannot be spared. Prof. Patric Walsh of Johns Hopkins University has repeatedly pointed out that the anatomy of the prostate and its surrounding structures is greatly simplified or simply misrepresented in most anatomy books – and little has changed in this regard to date2.

New developments:
Single-port transperineal robotic-assisted prostatectomy – the less invasive and less stressful alternative to Da Vinci surgery.
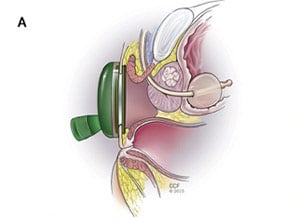
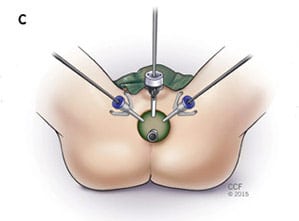
The modern advancement of the robotic-assisted da Vinci method, which requires multiple access points (ports) across the abdomen to the prostate (intraperitoneal), is the “single port” Da Vinci surgery, which uses one access route to the prostate without opening the abdomen (extraperitoneal). The approach via the pelvic floor is the gentlest3.
Initial studies have shown that transperineal extraperitoneal access with the surgical robot guarantees significantly faster patient recovery in addition to better cosmetic results. Avoiding the peritoneal access route avoids complications related to injury and blood supply disturbances to the small and large bowel, as well as problems with systemic absorption of CO2, a side effect that occurs when the abdomen is “inflated” with CO2 to displace the bowel during transperitoneal RARP.
However, the most important advantage of single-port transperineal RARP is the avoidance of the steep Trendelenburg position required by conventional transperitoneal RARP. This can prevent position-related cardiac, pulmonary, and neurological side effects.


Why be radical when you can be focal and gentle?
Radical operations used to abound. Women had their breasts cut off, and patients with kidney cancer had their kidneys removed. Famous and infamous became U.S. surgeon William Stewart Halsted, who was obsessed with curing women of breast cancer through increasingly radical surgeries. To do this, he removed not only the breast, but also parts of the chest wall and shoulder, and mutilated the affected women – unnecessarily, as it later turned out. Today, breast cancer is treated focally, by removing the cancer site while preserving the breast. And survival rates have gotten better, not worse. Also, in the case of kidney cancer, usually only the tumor and not the entire kidney is removed.
Only in the case of prostate cancer has the gentle focal removal of the cancer site while preserving the prostate not yet become established. One wonders why. There is no scientifically sound answer to this question.
It has long been known that radically cutting out cancer in healthy tissue cannot cure cancer. By the time the cancer site is discovered, individual cancer cells have been spreading from this site throughout the body for years, via blood and lymph vessels. This is the only way to explain the fact that after radical prostatectomy, after which the prostate cancer was removed from the body together with the prostate, recurrences and metastases occur years after the operation. And recurrences are common after radical prostatectomy, as can be read in the Johns Hopkins University HAN Tables
Irreversible electroporation
(IRE – NanoKnife)
However, developments in urology have not stood still either. Driven by developments in interventional radiology, increasingly gentler but no less effective focal therapies for prostate cancer have been developed in recent years.
The newest and currently most promising methods are so-called electroporation methods such as IRE (Irreversible Electroporation, NanoKnife®), with which prostate cancer can be treated without incontinence and in most cases without impotence.
