Protonentherapie
Modern radiotherapy with atomic nuclei
Proton therapy (PT) is a modern type of radiation therapy that uses accelerated protons instead of photons (X-rays or gamma rays) to irradiate and destroy malignant tumors. The main advantage of PT is the fact that the protons release their energy only after a certain depth of penetration into the body.
If this critical penetration depth is matched with the position of the tumor in the body, most of the energy will be released in the tumor and destroy it. On the way to the tumor, on the other hand, very little of its energy is released, which protects surrounding tissues from radiation damage.
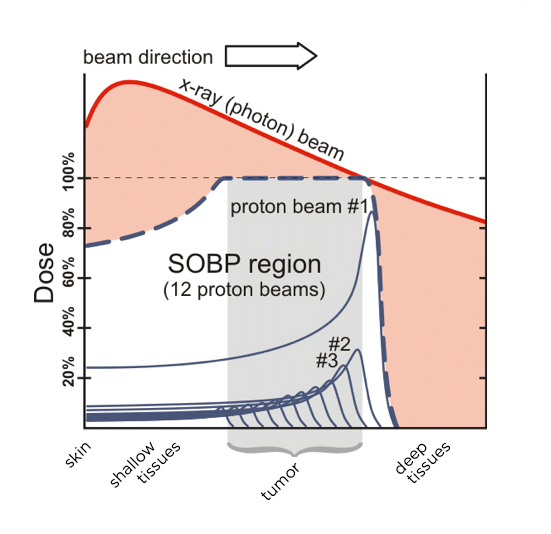
The red line shows the radiation dose distribution in conventional photon irradiation: here, the radiation dose is deposited for the most part outside the tumor, which leads to corresponding damage in the neighboring organs and tissues and can lead to new carcinomas in these2.
Proton therapy for prostate cancer:
Still the best process?
While proton therapy has important applications in childhood tumors, it is not ideally suited for the treatment of prostate cancer. This is because, in addition to optimized energy delivery, the precise focusing of radiation on the prostate is also important when irradiating the prostate.
Radiation therapy for prostate cancer:
Dynamic focusing with Cyberknife spares surrounding organs
The irradiation of prostate cancer with cyberknife (CN), a special type of photon therapy, has in the meantime proven to be more precise – and much less costly. While proton therapy requires up to 45 sessions, cyberknife can treat prostate cancer in as few as 5 sessions.
Radiation therapy as initial treatment for prostate cancer suboptimal
Im Allgemeinen ist jedoch die Strahlentherapie, unabhängig von der verwendeten Technik (iMRI = intensitätsmodulierte Strahlentherapie, PT, CN usw.), nicht die beste Wahl als Erstlinientherapie. This is because radiation therapy leaves genetic damage to the tissues that are in the marginal area of radiation. This results in chronic inflammation and severe scarring, especially in the area of the bladder and rectum when prostate cancer is irradiated. This chronic damage also reduces the ability of tissues to heal wounds, making further treatments in the radiation field much more difficult. Thus, further irradiations are usually not possible at all. The so-called “salvage” prostatectomy (rescue prostatectomy) is only performed by a few experts and results in pronounced incontinence in almost all cases. Since radiation therapies do not require anesthesia, they should be used primarily in old and sick men for whom anesthesia is too much of a burden.
The side effects of radiotherapy are similar to those of radical prostatectomy, with slightly lower rates of incontinence with RT than with RPE, but higher rates of bladder and bowel dysfunction3 (see Table).
RT
3,2%
4,4%
9,4%
RT
60,8%
71,9%
93,9%
bowel function
RT
34,0%
31,3%
35,8%
Table: Long-term consequences of radical prostatectomy (RPE) and radiotherapy (RT) for prostate cancer regarding incontinence, impotence, and impaired bowel function. Translated into German by Resnik MJ, Koyoma T, Fan K-H, et al. N Engl J Med 2013; 368:436-45.
Prostate cancer therapy almost without side effects
Electroporation process – without ionizing radiation
These side effects can be almost completely avoided by a new treatment method for prostate cancer, which no longer uses ionizing radiation, but ultra-short strong electrical pulses, the so-called“Irreversible Electroporation” (IRE), which was developed to application maturity at the VITUS Prostate Center.
