The radical prostatectomy
Still the standard of care for prostate cancer today
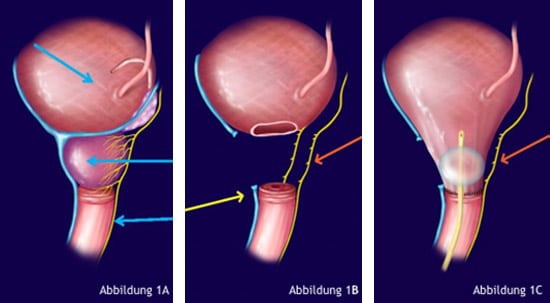
Radical prostatectomy is the standard treatment for prostate cancer. It describes the surgical removal of the entire prostate. In radical prostatectomy, the surgeon dissects free and removes the prostate gland, which lies below the urinary bladder and above the urethra and its sphincter.
To ensure the outflow of urine from the bladder, the base of the bladder must be sutured to the urethra or sphincter (see Figures 1A to 1C).
The most common side effects of radical prostatectomy are erectile dysfunction and urinary incontinence. These side effects are caused by damage to important anatomical structures during surgical removal of the prostate.
Erectile dysfunction results from damage to the so-called neurovascular bundle (NVB), a network of vessels and nerves that runs in and on the prostate gland and is responsible for penile erection.
Urinary incontinence, the involuntary loss of urine, is caused by damage to the sphincter of the urinary bladder; this is in fact a complex elongated structure that begins in the prostate and extends to the passage of the urethra through the pelvic floor.
In simple schematics of radical prostatectomy, the NVB is usually depicted as a “cable strand.” In reality, the NVB is an extremely complex network of small and tiny vessels and nerves in and on the prostate – and thus cannot be preserved during radical surgery. Figure 2A shows an anatomical preparation of the neurovascular network, also called “Aphrodite’s veil” because of its fine and diffuse structure. Figure 2B shows on a schematic cross-section through the prostate the different parts of the NVB and its course up and inside the prostate capsule.


Robotic Assisted Radical Prostatectomy (RARP).
(the DaVinci Procedure)
Since its introduction in 2000, robot-assisted radical prostatectomy (RARP) has increasingly replaced conventional open radical prostatectomy1.
However, this development was not spurred by the better results of RARP, but by “radical” marketing efforts by robotic system manufacturers and by hospitals that had installed a robotic system.

Many patients today are convinced that RARP is the better surgical method. However, this is by no means scientifically proven. While RARP may help to marginally reduce hospital stay and perioperative complications, several publications have pointed out the higher rates of impotence and incontinence after RARP.
In its publication2 “Prostate Knowledge”, Harvard Medical School concludes: Robot-assisted radical prostatectomy (RARP) is no better than open surgery. The best guarantee for low complication rates is the quality of the surgeon – not the robot!
How gentle is the RARP?
(the DaVinci Procedure)
To allow unobstructed access for the robotic arms to the prostate, the contents of the abdomen, primarily the small and large intestines, must be removed from the access path. This is done in Da Vinci surgery by turning the patient upside down. In this so-called “Trendelenburg” positioning, the patient and the operating table are brought to a head-down position of 45° (see Figure 4A). This is a considerable burden, especially for old, overweight and sick patients, in addition to the anesthesia, with an operation duration of 2 to 4 hours (without complications).
Stable positioning aids are necessary to fix the patient on the operating table to prevent him from sliding off the operating table. This can lead to nerve, joint and muscle injuries. Slippage of the patient leads to tears and postoperative hernias in the area of the inserted robotic arms. Muscle injury can lead to renal failure, cardiac arrhythmias, compartment syndrome, and persistent pain due to rhabdomyolysis. The head-down position can cause increased intraocular pressure, retinal detachment, and circulatory problems in the optic nerves, which can lead to blindness. In addition, the prolonged head-down position stresses the cardiovascular system and may cause swelling in the trachea, necessitating re-intubation after anesthesia.

Figure 4: A Positioning of the patient during RARP.
But what do existing clinical results of RARP application show? The recent work of Gardiner et al. published results3 which cover the first 12 weeks after RARP surgery and thus can initially only provide information on the short-term toxicity of the treatment. The physicians were able to show that the duration of surgery was shorter and intraoperative complications were less frequent, resulting in fewer unplanned admissions to the intensive care unit. There was also less blood loss. In addition, RARP patients were able to leave the hospital earlier than patients of regular prostate surgery. The results also showed that patients reported less pain one day after surgery and after one week. They also reported a higher quality of life compared with radical prostatectomy.
Regarding the effects on urinary continence and sexual function, the results were comparable in both groups at both six weeks and 12 weeks. Urinary continence tended to be better after conventional surgery, and robotic-assisted surgery had a slight advantage in sexual function. However, the differences were not found to be statistically significant.
Survival could not be compared in this study because the recorded time after therapy was too short for this. However, the proportion of positive marginal incisions after RARP was higher than for radical prostatectomy without robotic assistance, at 15 percent versus 10 percent. At the same time, twice as many lymph nodes (6.5 versus 3.26) were removed and the proportion of positive lymph nodes was significantly higher at 4 versus 1 percent. It therefore remains questionable whether the advantages of this therapy outweigh the disadvantages.
Alternatives to radical therapy?
Why be radical when you can be focal and gentle?
Radical operations used to abound. Women had their breasts cut off, and patients with kidney cancer had their kidneys removed. Famous and infamous became the U.S. surgeon William Stewart Halsted4, who was obsessed with curing women of breast cancer through increasingly radical operations. To do this, he removed not only the breast, but also parts of the chest wall and shoulder, and mutilated the affected women – unnecessarily, as it later turned out. Today, breast cancer is treated focally, by removing the cancer site while preserving the breast. And survival rates have gotten better, not worse. Also, in the case of kidney cancer, usually only the tumor and not the entire kidney is removed.
Only in the case of prostate cancer has the gentle focal removal of the cancer site while preserving the prostate not yet become established. One wonders why. There is no scientifically sound answer to this question.
That radically cutting out cancer in healthy tissue cannot cure cancer has long been known. By the time the cancer site is discovered, individual cancer cells have been spreading from it throughout the body for years, via blood and lymph vessels. This is the only way to explain the fact that after radical prostatectomy, after which the prostate cancer was removed from the body together with the prostate, recurrences and metastases occur years after the operation. And recurrences are common after radical prostatectomy, as can be seen in the Johns Hopkins University HAN Tables.
However, developments in urology have not stood still either. Driven by developments in interventional radiology, increasingly gentler but no less effective focal therapies for prostate cancer have been developed in recent years . The newest and currently most promising methods are so-called electroporation methods such as IRE(Irreversible Electroporation, NanoKnife®), with which prostate cancer can be treated without incontinence and in most cases without impotence.
