Stereotactic body radiotherapy (SBRT) with the Cyberknife
Conventional radiotherapies of the prostate are characterised by repeated irradiations, each with a low dose, because the radiation cannot be sufficiently focused on the prostate. Thus, the surrounding tissue, especially the intestine and the urinary bladder, is also damaged by the radiation. To keep side effects low, the total dose is divided into up to 45 “fractions”. This means that the patient needs up to 45 radiotherapy appointments, with daily therapy sessions for a total of up to 9 weeks.
Unlike many other cancers, however, prostate cancer responds particularly well to a few high-dose irradiations. Due to the much better focus on the prostate, SBRT with the Cyberknife allows the total dose to be applied in only 5 sessions – with less damage to the surrounding organs. Each session lasts about 15 to 30 minutes.
In this way, cybernife irradiation has in the meantime surpassed even proton therapy in terms of precision.
Robot-guided radiation source delivers sharp dose gradients
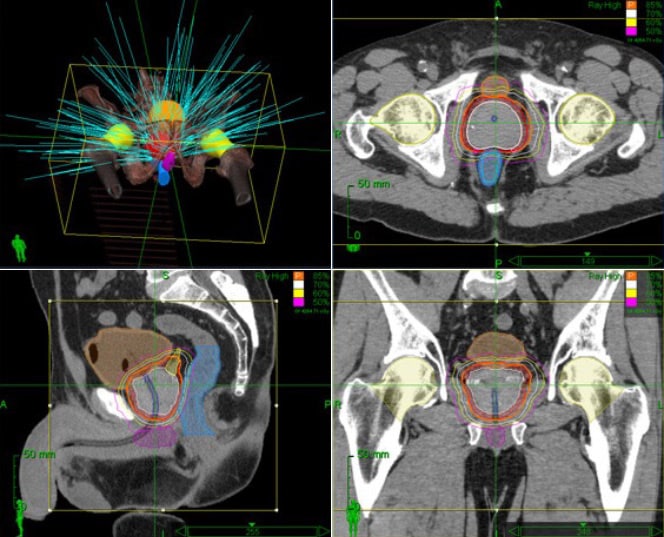
The Cyberknife differs from radiation therapy systems in that a conventional radiation source (high-energy photons) is attached to an industrial robot system, and thus freely movable in space. This allows a tumour in the patient’s body to be irradiated from all spatial directions with a sharply focused beam (“pencil beam”).
The CyberKnife’s robotic system thereby seamlessly delivers non-coplanar, non-isocentric and isocentric beams from a variety of angles. These unique delivery options generate conformal dose distributions and enable precise and effective treatments.
Of particular importance are the sharp dose gradients that are typical of the cyberknife. Because ideally, the tumour should be hit with maximum radiation dose, and the surrounding tissue with a dose of zero. Of course, this ideal dose distribution can never be achieved. But dropping as quickly as possible from the maximum dose in the tumour (e.g. 80 grays) to very low doses of 2-5 grays within a transition zone only 1 – 2 cm wide minimises the radiation dose to surrounding organs such as the bladder, rectum and nerves and vessels.
Cyberknife (SBRT) irradiation procedure
SBRT consists of a much shorter course of radiation than conventional approaches, with only five treatment sessions. This is achieved by administering a higher dose per day, which requires considerable precision and accuracy, drawing on the expertise of the treating radiation oncologist and a team of medical physicists, medical dosimetrists and radiotherapists. Modern and advanced linear accelerator technology is also required. A total of six visits to the department are required for the planning and implementation of SBRT (one planning visit and five treatment visits).
Motion and image-guided radiotherapy of the prostate gland
Because the prostate can move due to the filling and emptying of the bladder and rectum, SBRT requires a high degree of accuracy. To ensure that the prostate is accurately targeted and tracked, we place 3 implanted markers (called fiducials) in the prostate. All our treatment units are equipped with onboard X-ray imaging devices or cone beam CT technology, which allows these markers to be tracked as the prostate moves. In addition, a cone beam CT is performed before each treatment session to ensure that the anatomy is stable for treatment. This generally means a full bladder and an empty rectum. We provide each patient with detailed instructions on how to prepare for treatment.
Including all of these imaging steps, SBRT for prostate cancer with the UCLA protocol takes only 15 minutes per treatment session, using state-of-the-art RapidArc treatment techniques. Since images are used to guide the treatment, the term “IGRT” or “image-guided radiotherapy” can be used when referring to the precision with which SBRT is performed.Scans for radiation planning
In order to be able to actually deliver radiation, individual radiation planning must be carried out after the implanted markers have been placed. This is a special high-resolution CT that must be performed in the Department of Radiation Oncology at UCLA. It is not a diagnostic scan. Technically, it is a CT simulation scan.
As the prostate is much better visualised on an MRI than on a CT scan, we also try to get an MRI scan to help with treatment delineation as well. Sometimes an MRI has already been done during the diagnosis of prostate cancer, and this might be sufficient. In other cases, a new MRI is recommended.Irradiation planning procedure
After the CT simulation examination (±radiation planning MRI), your radiation oncologist will draw up an individual radiation plan together with a team of medical physicists and a medical dosimetrist. This process usually takes five working days.SBRT delivery
The treatment itself takes place over the course of five treatments. These are usually carried out every second working day. Each treatment itself takes 15 minutes (including the imaging scans discussed above). The treatment is carried out with high-energy, invisible X-rays.
Advantages of Cyberknife (SRBT) irradiation
There are many good reasons to consider cyberknife radiation (SBRT). Advantages over conventional radiotherapy include:
- Cyberknife radiation is completely non-invasive (unlike brachytherapy, it does not involve the insertion of needles, bleeding risks, risk of infection, general anaesthesia, hospitalisation or wearing a catheter).
- Cyberknife radiation has a significantly shorter treatment duration than conventional external beam radiation therapy, which can last up to 9 weeks. SBRT of the prostate requires only t 5 treatment sessions of about 15 minutes each, all of which can be performed on an outpatient basis.
- The cancer control rates of SBRT are equivalent to those of brachytherapy, conventional external beam radiotherapy and surgical removal of the prostate.
- The sparing of radiation exposure to the rectum and bladder is equal to or better than brachytherapy.
Synchronisation of movement in real time
The revolutionary Synchrony® system uses artificial intelligence to adapt the treatment to the movements of the patient and/or target in real time without human intervention. At the touch of a button, CyberKnife S7™ treatments can be performed continuously, efficiently and without interrupting standard workflows.

Disadvantages of radiotherapy
Im Allgemeinen ist jedoch die Strahlentherapie, unabhängig von der verwendeten Technik (iMRI = intensitätsmodulierte Strahlentherapie, PT, CN usw.), nicht die beste Wahl als Erstlinientherapie. This is because radiation therapy leaves genetic damage to the tissues that are in the marginal area of radiation. This results in chronic inflammation and severe scarring, especially in the area of the bladder and rectum when prostate cancer is irradiated. This chronic damage also reduces the ability of tissues to heal wounds, making further treatments in the radiation field much more difficult. Thus, further irradiations are usually not possible at all. The so-called “salvage” prostatectomy (rescue prostatectomy) is only performed by a few experts and results in pronounced incontinence in almost all cases. Since radiation therapies do not require anesthesia, they should be used primarily in old and sick men for whom anesthesia is too much of a burden.
The side effects of radiotherapy are comparable to those of radical prostatectomy, although the incontinence rate is slightly lower with RT than with RPE, but the disruption of bladder and bowel function is higher1.
NanoKnife treatment
The gentle alternative to radiotherapy
These side effects can be almost completely avoided by a new treatment method for prostate cancer that no longer uses ionising radiation, but ultra-short, strong electrical pulses, the so-called “Irreversible Electroporation (IRE)“, which was developed to application maturity at the VITUS Prostate Centre.
RT
3,2%
4,4%
9,4%
RT
60,8%
71,9%
93,9%
bowel function
RT
34,0%
31,3%
35,8%
Table: Long-term consequences of radical prostatectomy (RPE) and radiotherapy (RT) for prostate cancer regarding incontinence, impotence, and impaired bowel function. Translated into German by Resnik MJ, Koyoma T, Fan K-H, et al. N Engl J Med 2013; 368:436-45.
