Stage 4 (Metastasised) Prostate Cancer
Prostate cancer is one of the most prevalent cancers among men, often detected in its early stages when treatment options are most effective. However, when prostate cancer advances to stage 4, it becomes a much more serious and complex disease. At this stage, the cancer has metastasized, or spread, beyond the prostate gland to other parts of the body. This article explores the nature of prostate cancer metastasis, the limitations of traditional treatment methods, and the promising role of focal therapy and immunotherapy in managing and potentially reversing this advanced stage of the disease.
What Is A Prostate Cancer Metastasis?
Metastasis refers to the process by which cancer cells break away from the primary tumor in the prostate and travel through the bloodstream or lymphatic system to establish new tumors in other parts of the body. In stage 4 prostate cancer, metastases most commonly occur in the bones, lymph nodes, liver, and lungs. Bone metastases are particularly common and can lead to severe pain, fractures, and other complications that significantly impact a patient’s quality of life. When prostate cancer spreads to organs such as the liver or lungs, it can interfere with their function, causing symptoms such as jaundice or respiratory difficulties.
How Fast Does Prostate Cancer Metastasize?
The rate at which prostate cancer metastasizes varies significantly among individuals. Factors such as the Gleason score (which measures the aggressiveness of the cancer), the patient’s overall health, and the presence of specific genetic markers all play a role in determining how quickly the cancer spreads. High-grade tumors with higher Gleason scores are generally more aggressive and more likely to metastasize rapidly compared to low-grade tumors. In some cases, prostate cancer may remain localised for many years, while in others, it may spread quickly to distant sites.
How is metastasised prostate cancer treated?
Traditional Treatments and their drawbacks
Historically, the primary treatment options for stage 4 prostate cancer have included surgery, radiation therapy, hormone therapy, and chemotherapy. While these treatments can be effective in reducing the size of tumors and controlling the spread of cancer, they are not without significant drawbacks:
- Chemotherapy: Chemotherapy uses powerful drugs to kill rapidly dividing cells, including cancer cells. However, it is a blunt tool that also affects healthy cells, leading to a host of debilitating side effects such as nausea, hair loss, fatigue, and an increased risk of infection. Chemotherapy’s effectiveness in treating metastatic prostate cancer is limited, and it often comes with a significant toll on the patient’s overall health and quality of life.
- Surgery (Radical Prostatectomy): Surgery involves the removal of the prostate gland and surrounding tissue. Although it can be effective in removing the primary tumor, surgery is highly invasive and often comes with a risk of serious side effects, including incontinence and sexual dysfunction. Additionally, surgery is not typically an option for treating metastases that have spread beyond the prostate.
- Radiation Therapy: Radiation therapy uses high-energy rays to target and kill cancer cells. While it can be effective in reducing the size of tumors, it also damages surrounding healthy tissue. This collateral damage can lead to significant side effects, including fatigue, urinary problems, and gastrointestinal issues. Radiation therapy is also limited in its ability to treat metastases effectively, particularly when cancer has spread to multiple sites.
- Hormone Therapy: Hormone therapy aims to reduce the levels of androgens (male hormones) that prostate cancer cells need to grow. Although hormone therapy can slow the progression of the disease, it is not a cure and often comes with severe side effects, including loss of libido, hot flashes, and an increased risk of cardiovascular disease. Moreover, many prostate cancers eventually become resistant to hormone therapy, rendering it ineffective.
Focal Therapy and combined Immunotherapy: Innovative Approaches to Metastatic Prostate Cancer
Given the limitations and significant side effects associated with traditional treatments, there is a growing interest in less invasive, more targeted approaches to managing metastatic prostate cancer. Two of the most promising approaches are focal therapy and immunotherapy.
Focal Therapy: Precision Targeting of Cancer Cells
Focal therapy is an innovative treatment approach that targets specific areas of the prostate affected by cancer while sparing the surrounding healthy tissue. Unlike traditional treatments, which often involve treating the entire prostate gland (and sometimes beyond), focal therapy aims to destroy only the cancerous tissue. The most common forms of focal therapy include:
- Irreversible Electroporation (IRE): IRE, also known as NanoKnife, is a cutting-edge focal therapy that uses electrical pulses to create tiny pores in cancer cell membranes, leading to cell death without the use of extreme heat or cold. This technique is particularly effective because it preserves the surrounding structures, such as nerves and blood vessels, that are often damaged by other treatments. IRE can be used to treat both localized prostate cancer and certain metastases, especially those in sensitive areas where precision is crucial.
- Cryotherapy: This technique uses extreme cold to freeze and destroy cancer cells. Cryotherapy is minimally invasive and can be repeated if necessary. It is particularly effective for localized prostate cancer but may also be used in certain cases to target metastases.
- High-Intensity Focused Ultrasound (HIFU): HIFU uses focused sound waves to generate heat, which destroys cancer cells. This method is also minimally invasive and offers the benefit of being highly precise, minimising damage to surrounding tissue.
- Laser Ablation: Laser ablation involves using concentrated light to destroy cancer cells. It is another targeted, minimally invasive option that is effective for treating localized tumors.
While focal therapy is highly effective for localised prostate cancer, its application to metastases is more limited. Metastatic sites are often dispersed and may involve organs or bones that are difficult to treat with localised therapies. However, focal therapy can still play a role in managing certain metastases, particularly in combination with immunotherapy amongst other treatments.
The Synergy Between Focal Therapy and Immunotherapy
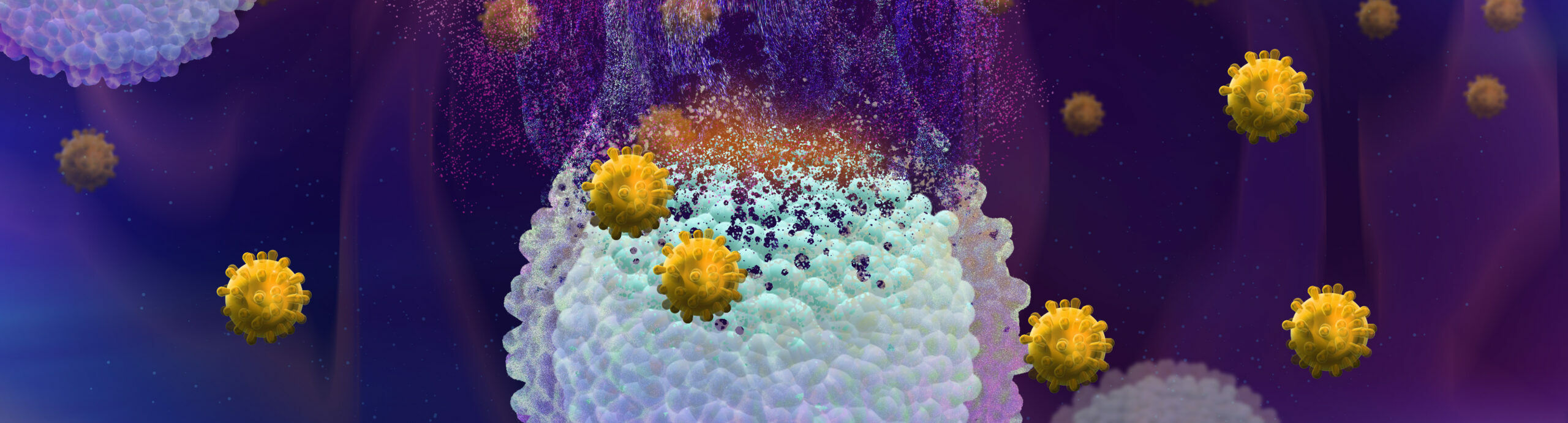
One of the most promising strategies in the treatment of metastatic prostate cancer is the combination of focal therapy and immunotherapy. The synergy between these two approaches is based on a critical aspect of cancer biology: the release of cancer antigens.
When focal therapy, such as IRE or HIFU, targets and destroys prostate cancer cells, it causes the release of cancer antigens into the bloodstream. These antigens are essentially the “fingerprints” of cancer cells—unique markers that the immune system can recognize. However, on their own, these antigens may not be sufficient to trigger a strong immune response.
This is where immunotherapy comes into play. By using immunotherapy agents, such as immune checkpoint inhibitors (e.g., Keytruda), the immune system can be “trained” to recognize and attack cancer cells throughout the body, including metastases. Keytruda (pembrolizumab) works by blocking a protein called PD-1, which prevents immune cells from attacking cancer cells. When combined with the antigen release from focal therapy, Keytruda can enhance the body’s ability to target and destroy metastatic cancer cells that would otherwise go undetected.
This combination approach is particularly exciting because it turns the body’s natural defense system into a more effective weapon against cancer. By leveraging the precision of focal therapy and the systemic effects of immunotherapy, patients may experience better outcomes with fewer side effects compared to traditional treatments.
Experimental Approaches: Targeting Metastases with Immunotherapy and Chemotherapeutic Agents
In treating metastatic prostate cancer, combining chemotherapeutic agents with immunotherapy is an exciting experimental approach that aims to make cancer cells more visible to the immune system. Chemotherapy drugs like docetaxel not only kill cancer cells but also help release signals and antigens that alert the immune system, making it easier for immunotherapy drugs, like Keytruda, to recognize and attack these cells.
At our clinic, we take this a step further by carefully timing and targeting the treatment:
- Two weeks before focal therapies like IRE (Irreversible Electroporation), we administer a dose of docetaxel and ipilimumab (Yervoy) directly into the prostate (or lymph node metastases). This primes the immune system by making the cancer cells more recognizable.
- One day before the ablation therapy, we give two doses of Keytruda to boost the immune response.
- After the ablation, three weeks later, another dose of Keytruda is administered to ensure the immune system continues to target any remaining cancer cells.
This approach helps to maximize the effectiveness of the treatment by combining the power of localized chemotherapy and immunotherapy with precision-targeted focal therapies and was able to completely erradicate one of our patient’s lymph node metastases (even though only one was injected with the chemo– and immunotherapeutic agents).
Interested in Immunotherapy? We’re here to help.
The Future of Treating Prostate Cancer Metastasis
The treatment of stage 4 prostate cancer metastasis is complex and requires a personalized approach that considers the unique characteristics of each patient’s disease. While traditional treatments like surgery, radiation, hormone therapy, and chemotherapy have played a significant role in managing the disease, they come with substantial drawbacks that can affect a patient’s quality of life.
In contrast, focal therapy and immunotherapy offer promising alternatives that may provide effective treatment with fewer side effects. Focal therapy’s ability to target specific areas of cancer while sparing healthy tissue, combined with immunotherapy’s potential to harness the body’s immune system to fight cancer, represents a new frontier in the treatment of metastatic prostate cancer.
However, it’s important to note that these newer therapies are not yet a complete replacement for traditional treatments. In some cases, particularly when dealing with widespread metastasis, a combination of therapies may be necessary. Ongoing research and clinical trials continue to explore the most effective ways to integrate these innovative treatments into a comprehensive strategy for managing advanced prostate cancer.
conclusion
Stage 4 prostate cancer metastasis remains a formidable challenge, but advancements in focal therapy and immunotherapy offer new hope for patients. The synergy between these treatments, particularly the combination of focal therapy and immunotherapy, represents an exciting development in cancer treatment. While traditional treatments have their place, particularly in specific scenarios where metastasis is widespread or inaccessible to newer therapies, the future of prostate cancer treatment lies in approaches that minimise harm while maximising effectiveness. Patients and their healthcare providers should work together to explore all available options, tailoring treatment strategies to the individual needs of each patient. Connect with our medical experts for a detailed assessment of your treatment options and take the first step toward a personalized care plan.
By staying informed about the latest advancements and understanding the full spectrum of treatment options, patients can make empowered decisions that align with their personal goals and overall well-being.