Targeted biopsies – MRI-guided biopsy of the prostate
If prostate cancer is suspected, a biopsy is often the next step after the initial examinations. Biopsy procedures in which foci that are conspicuous in a previous magnetic resonance imaging of the prostate are targeted and biopsied have a better accuracy. These biopsies are called MRI-guided or targeted biopsies. They increase the accuracy of the biopsy to 60-70%; still almost twice as good as TRUS biopsy. This is because more than 50% of all prostate cancer foci that are conspicuous on MRI are not visible on ultrasound.


Why MRI/US fusion biopsy doesn’t work

Biopsy procedures in which foci that are conspicuous in a previous magnetic resonance imaging of the prostate are targeted and biopsied have a better accuracy. These biopsies are called MRI-guided or targeted biopsies. They increase the accuracy of the biopsy to 60-70%; still almost twice as good as TRUS biopsy. This is because more than 50% of all prostate cancer foci that are conspicuous on MRI are not visible on ultrasound.
The best known is the so-called MRI/US fusion biopsy, in which the MRI images of the prostate are overlaid – fused – with the real-time ultrasound images acquired during the biopsy. And therein lies the problem. While MRI images rigidly reflect the anatomy of the prostate during the MRI exam, the prostate is constantly changing shape during a biopsy. This is because the prostate has soft and hard parts and is both elastic and plastically deformable. Therefore, the MRI images and US images do not match.
So-called elastic fusion algorithms have been used to try to solve this problem. Without success. Therefore, actual fusion biopsy is increasingly being replaced by so-called “cognitive” fusion biopsy, in which the tumor focus is localized in the MRI image and then localized by measurement in the US image.
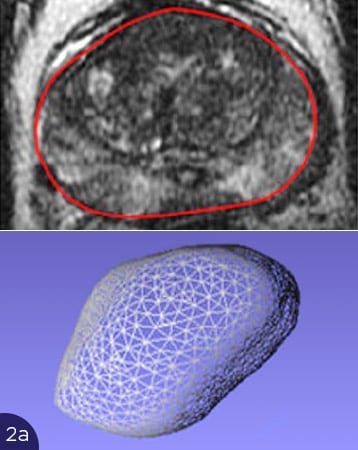

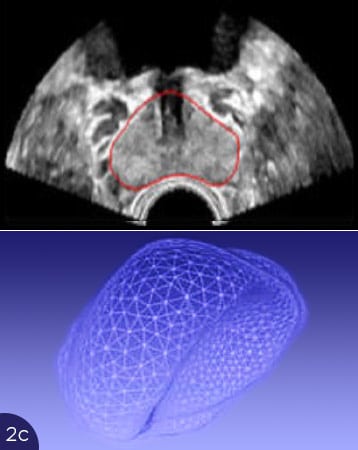

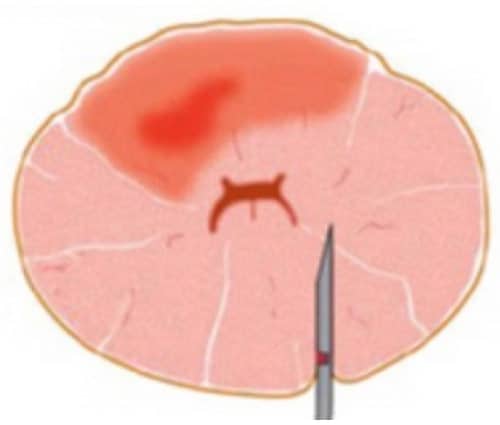
The figures show the problems with overlaying US and MRI images. In fig. 2(a), the shape of the prostate is shown in the MRI image, above as a cross-section (red border), below as a 3D representation of the entire prostate. In fig. 2b to 2d are cross-sections of the prostate on ultrasound (top, red outlines), and the corresponding 3D volumes are shown below. Depending on the filling of the bladder or pressure of the ultrasound transducer in the rectum, the prostate deforms strongly. Matching the MRI cross-section is not achievable. Thus, correct superimposition of the US and MRI images is not possible. A carcinoma focus would show up in a different location on the ultrasound than on the MRI image, and a targeted biopsy would not be possible.

MRI-guided robotic-assisted biopsy of the prostate gland
The problems of fusion biopsy and invisibility of cancer foci on ultrasound can be elegantly avoided if the biopsy is performed directly MRI-guided in the MRI scanner itself.
At Vitus Private Clinic, we use this option of precise biopsy guided directly by MRI images. For this purpose, the biopsy needle is steered into the suspicious focus either manually or with a Soteria biopsy robot, under direct MRI control. This makes it possible, with high precision, to steer the biopsy needle directly into the suspicious focus in the prostate. Once there, the biopsy can be followed directly on MRI, and after sampling, imaging of the stitch canal can verify that the focus was hit. In this way, even small carcinoma foci can be biopsied with a high degree of certainty2.




3D mapping biopsy
Highest accuracy and localization diagnosis before focal therapy

3D mapping biopsy, also called “template” biopsy, provides even more reliable and accurate results. It is performed mainly in the U.S. in patients who choose “Active Surveillance” for their prostate cancer – or focal therapy.
Mapping biopsy detects carcinoma of the prostate with 80 – 100% accuracy.
In addition, it is the only biopsy method that provides accurate information about the spatial distribution of cancer foci in the prostate, as each individual biopsy is obtained using a three-dimensional coordinate system, so that each sample can be assigned an x, y, and z coordinate. Biopsy samples are collected through a brachytherapy grid, a perforated plate that has a hole every 5 mm.
This is superimposed on the pelvic floor of the prostate and the holes are displayed on the ultrasound screen. The biopsy needle is now inserted into the prostate through the holes superimposed on it. In this way, the prostate is systematically biopsied every 5 mm, which may result in 30 to 60 samples, depending on the size of the prostate (in very large prostates, the number of samples is reduced).
3D mapping biopsy should only be performed in patients seeking focal treatment. Only in this case it is necessary to obtain information about the distribution pattern of carcinoma in the prostate. This is not necessary with radical therapies, as these involve the removal or destruction of the entire prostate.
Call us now on +49 (0)177 23 82 863 or get in touch using the contact form
How does the TRUS biopsy work?
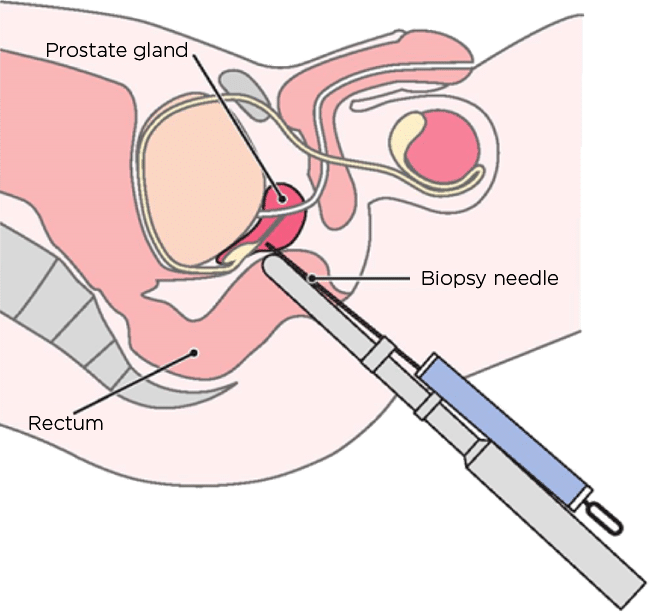

During TRUS biopsy, 12 tissue samples are usually taken from the prostate under ultrasound guidance. The biopsy needle is inserted into the prostate through the rectum (rectal – hence transrectal – through the rectum). In this process, germs (bacteria) are carried from the rectum into the prostate.
In about 20% of men, TRUS biopsy is followed by infection of the prostate (prostatitis), which must be treated with antibiotics.
Recent statistics show that 1 to 2 of every 1000 men (0.1-0.2%) who have undergone transrectal biopsy die from antibiotic-resistant germs carried from the intestine to the prostate. And the trend is upward.
However, TRUS biopsy has other disadvantages: In 100 men with prostate cancer, TRUS biopsy finds the carcinoma in only 30-40 men. With the others it is not hit. For this purpose, TRUS biopsy often hits clinically insignificant cancer foci that are not considered worthy of treatment. Because: Already at the age of 60 years every second man has small, but for the health of the man insignificant cancer foci in the prostate, at the age of 80 years in 90% of all men!
Today, magnetic resonance imaging (MRI) of the prostate has twice the accuracy for detecting or excluding clinically relevant carcinomas as TRUS biopsy. Therefore, TRUS biopsy should actually no longer be performed – but it remains the standard biopsy listed in the S3 guideline!
TRUS prostate biopsy about to be banned?
In Germany, however, still standard according to S3 guideline.
According to the S3 Guideline Prostate Cancer of the German Society of Urology, TRUS biopsy, transrectal (performed through the rectum) ultrasound-guided punch biopsy, continues to be the standard biopsy for elevated PSA levels or abnormal magnetic resonance imaging (MRI) of the prostate.
Nevertheless, several countries in the EU are currently discussing banning TRUS biopsy.
Why? Because TRUS biopsy is performed through the rectum, it often results in prostate infections. Antibiotic-resistant germs cause 1 -2 of 1000 men to die after a TRUS biopsy.
Diagnostics – Frequently Asked Questions (FAQ)
The so-called Gleason score is a measure of the aggressiveness of prostate cancer. It results from the microscopic sections that the pathologist prepares from the biopsy specimens. The Gleason score is an elementary component of the so-called grading (classification into differentiation grades) of prostate carcinoma. In addition to grading, staging (staging, TNM classification) is always required, preferably by MRI.
Somewhat simplified, we can summarize:
Gleason score 3+3 = 6
Rarely, prostate cancer with this Gleason score is high risk.
The 10-year survival probability is over 99%.
If this Gleason score is exclusively present, Active Surveillance, Watchful Waiting, or sparing focal therapy with IRE/NanoKnife should be considered. Radical therapies bring no survival benefit here, but many unnecessary side effects. Let us advise you.
Gleason score 3+4 = 7a
The most common Gleason score. Prostate cancer with this Gleason score is intermediate risk.
Mortality risk here is strongly dependent on PSA level and spread.
Therapy should be considered here. Both focal and radical therapies make sense here.
This makes perfect diagnosis and counseling all the more important for this Gleason score.
Statistically, radical therapies are most effective at the intermediate Gleason score (= reduction of prostate cancer specific mortality). Let us advise you.
Gleason score 4+3 = 7b
Similar to Gleason score 7a, but with predominant load to the riskier 4 pattern.
Often the evaluation between 7b and already 8 is difficult and very pathologist-subjective.
Propagation estimation (also by MRI) is very important here.
Gleason score 4+4 = 8
From here on, one always speaks of a high-risk prostate carcinoma (regardless of age or PSA value).
Although the probability of survival over 10 years is still high (compared to other cancers), this prostate cancer usually has a high impact on the patient’s life expectancy.
In particular, the risk of recurrence after successful prostate cancer treatment is high here.
Anti-hormonal therapy may be necessary/recommended.
Gleason score 4+5 = 9 and 5+5 = 10
These highest Gleason scores are typically found in advanced carcinomas.
The probability that the carcinoma has already formed (micro-)metastases is significantly higher.
Good advice is also absolutely essential here.
Adjuvant (=supportive) therapies in addition to primary therapy are not unlikely here. E.g. anti-hormonal therapy or more recently immunotherapies.
In the following document we explain in more detail:
How does the risk of dying from prostate cancer relate to the Gleason score?
How does the likelihood of developing a recurrence relate to the Gleason score?
Prostate cancer information on treatment efficacy, cure rate and survival probability.
Important for the patient:
The Gleason score is a subjective evaluation. As such, this is subject to intrinsic imprecision. Therefore, while it is a good approximation, it is never an exact measure that can accurately predict a patient’s individual risk.
In addition to the Gleason score, it is equally important how many samples were positive and, most importantly, what spread the MRI of the prostate shows. This dispersion estimation is called staging. Grading and staging together are the first necessary steps before any therapy for any carcinoma.
An MRI is a non-invasive, painless method of medical imaging. Examinations can thus be performed without radiation exposure. An MRI allows 3D images to be taken as well as a variety of physical diagnostic parameters to be collected. Combined, these parameters allow exceptionally reliable statements to be made about the tissue properties at a specific site within the prostate – for example, in the case of carcinoma. An MRI is an effective method of medical imaging for prostate examination and should be performed as soon as possible in the case of suspected prostate cancer.
An MRI scan also shows the extent of the prostate cancer and provides information on whether the tumor is limited to the prostate or has already spread to surrounding structures (staging). This is a very important factor when weighing the various treatment options. MRI is considered superior to other methods such as ultrasound, histoscanning, elastography, CT (computed tomography), and PET/CT (positron emission tomography with CT). For optimal results, an MRI scan of the prostate should be performed at 1.5 or 3.0 Tesla using an endorectal coil.
Advances in the development of MRI examinations have meant that the procedure can now be performed as a whole-body examination. Thus, MRI replaces both bone scintigraphy and CT scans as staging tools for secondary metastases and affected lymph nodes. Completely free of exposure to ionizing radiation, MRI offers increased accuracy and reduces the examination time from four to six hours for bone scintigraphy to about one hour.
Contact us.
First, we would recommend an MRI scan of the prostate, followed by either an MRI-guided biopsy or a 3D biopsy, depending on whether one or more abnormal sites were detected.
Contact us.
For best results, an endorectal coil should be used during the MRI scan (even at 3 Tesla). However, often the results of an investigation at 3 Tesla are worse than at 1.5 Tesla. This is because the stronger magnetic field leads to an increase in susceptibility artifacts (image distortions) and higher energy deposition (SAR – specific absorption rate).
The endorectal coil must be filled with a susceptibility-neutral substance. Furthermore, the calculation and interpretation of many parameters, such as diffusion, perfusion, and MR spectroscopy, is highly complex. There are only a few specialists who have the necessary expertise to do this.
Contact us.
We recommend a transperineal 3D (histology mapping) biopsy instead of a transrectal punch biopsy. Because this method significantly reduces the risk of infection. This is because samples are obtained under sterile conditions through the skin of the perineum and not through the wall of the rectum. The examination is performed under general anesthesia.
3D biopsy has an accuracy of 80 to 100 percent in detecting carcinoma. With a conventional transrectal punch biopsy, the figure is only 30 to 35 percent. The 3D biopsy also provides a reliable Gleason score and an accurate map of how the cancer is distributed within the prostate. It is very rarely necessary to repeat this type of examination.
Contact us.
For the exclusion and localization of clinically relevant prostate carcinoma: yes.
When determining the tissue (carcinoma type/grade): only conditionally.
Both diffusion and 1H MR spectroscopy can provide clues to the aggressiveness of a carcinoma. Only histopathological analysis of tissue samples obtained by biopsy can confirm this evidence. The findings obtained from this are documented as a Gleason score.
However, biopsy alone cannot replace MRI examination. MRI allows the detection and localization of cancerous tissue so that it can then be selectively biopsied to obtain cancerous tissue for histopathologic examination. This allows the degree and size (staging and grading) of the tumor to be determined.
In some cases, after an MRI, the biopsy can be skipped and therapy can be started directly. However, these are isolated cases which can only be discussed after a thorough anamnesis in the tumor board.
Contact us.
Transrectal biopsies involve taking between six and twelve samples through the rectum, either blindly or with the aid of ultrasound. The accuracy of a transrectal biopsy is 30 to 35 percent, even when the number of samples taken is increased to a maximum of 24. Considering the respective sample size (< 1 millimeter in diameter, 10 to 25 millimeters in length), it becomes clear that in fact only tissue is taken from a small area of the prostate. If the tumor is not in the biopsied areas, no cancerous tissue is collected.
Transrectal biopsies are performed by inserting a biopsy needle into a predetermined area of the prostate. The exact origin of the sample cannot be determined in this process (accuracy of only five to 10 cubic centimeters), since no coordinate system is used during tissue sampling. In addition, not all areas of the prostate can be easily biopsied due to the narrow conditions in the rectum and the angle of insertion required by the biopsy needle. In addition, during the transrectal procedure, each biopsy needle carries fecal matter into the prostate. The associated increasing risk of prostatitis (inflammation of the prostate) limits the number of biopsies that can be performed. Whether the samples taken with this technique contain cancer cells ultimately depends on chance.
Transperineal biopsy, on the other hand, uses a more anatomically precise method to obtain specimens and comes to an accuracy of origin of 0.5 to 1 cubic centimeter. With this method, samples can be localized five to twenty times more precisely than with a transrectal biopsy. It also allows access to all areas of the prostate. There is also no risk of contamination with feces here.
Despite these statistics, transrectal biopsy still has its place in the diagnosis of large carcinomas (tumors). Prior to radical prostatectomy, it is sufficient to confirm carcinoma based on a positive specimen before surgically removing the prostate. However, gentler, focal therapy requires a great deal of site information that a traditional biopsy cannot provide. This information is obtained by 3D histology mapping biopsy. A 3D histological model of the prostate then helps in treatment planning and allows for precise treatment in which only the cancer cells are targeted and destroyed.
Contact us.
Advantages:
Precise
No risk of infection
Minimal postoperative pain and bleeding
Performed under general anesthesia
3D model of the prostate
Disadvantages:
Due to the complex planning and precise execution, this diagnostic technique is more expensive than regular biopsies.
It is also possible to perform targeted MRI biopsies (MRI-targeted biopsies or fusion biopsies). However, these serve a different purpose: it involves confirming a carcinoma for subsequent radical therapy rather than planning focal therapy.
Contact us.
In order to select the best treatment, the spread and type of carcinoma (tumor) should be known precisely. This is called staging and grading.
Staging:
Distribution of carcinoma within the prostate.
Spread of carcinoma outside the prostate to other organs in the pelvis (seminal vesicles, pelvic floor, etc.)
Spread of carcinoma to other organs, lymph nodes, and/or bone.
Grading:
Histological appearance of the carcinoma
Carcinoma type
Aggressiveness of the tumor
Person-related factors are also taken into account:
Patient age
General health
Sexual and general activity
Prostate size
PSA values
Once all these parameters have been identified, they can be used to select the most appropriate treatment from a wide range of options:
Watch and wait – active surveillance (Active Surveillance)
Focal therapy: NanoKnife, HIFU, laser, RFA, etc.
Partial or radical prostatectomy
Brachytherapy, afterloading, CyberKnife, proton radiotherapy, conventional radiotherapy, etc.
Hormone blockade
Chemotherapy
Immunotherapy
We will be happy to advise you on both conventional and modern therapy methods.
Don’t worry: Because the prostate, and therefore prostate cancer, typically grows slowly, you have plenty of time to gather comprehensive information and expert opinions. The goal of any therapy should be to control prostate cancer while avoiding complications such as impotence, incontinence, or radiation damage.
Together, we can develop a strategy that provides the optimal diagnosis and treatment for your prostate cancer.
Contact us
You should clarify the question of which costs are covered directly with your statutory health insurance. However, the cost of endorectal MRI and 3D biopsy is not covered by health insurance.
Even if you have private health insurance, we recommend that you clarify exactly which costs for diagnostics and therapy your health insurance will cover before you have a procedure performed. We will be happy to provide you with information on this.
Contact us.
The cost of both multiparameter MRI and 3D biopsy is highly dependent on the individual case.
Contact us to get an accurate assessment for your specific case.


